The Brainstem
In 5 Levels of Complexity
Introduction and Overview
This page is designed to introduce the anatomy of the brainstem in five building levels of complexity. Each level assumes knowledge of the previous level. When presented with all the details at once, it is easy to be overwhelmed. The idea behind the layout of this page is to avoid this and to facilitate learning the structures in an efficient order.
User guide:
New structures are written in purple and recurring structures are dimmed.
Images with a yellow bar underneath are stacks of images that can be scrolled or clicked on desktop and tapped on mobile. Scroll through the adjacent stack to get a preview of some of the structures that will be covered by level 5.
Starting at level 3, use the toggle labels button to review structures covered in the previous levels or to declutter the image.
Each level can be collapsed using the minimize / maximize buttons on the right of the screen.
Use the toggle outline button in the top left to navigate the page. Make sure the level you are trying to skip to is not minimized.
Level 1
- Midbrain
- Pons
- Medulla
- Interpeduncular cistern
- Cerebral aqueduct
- Periaqueductal gray matter
- Fourth ventricle
- Basilar artery
- Internal auditory canal
- Median aperture
- Vertebral arteries
- Cisterna magna
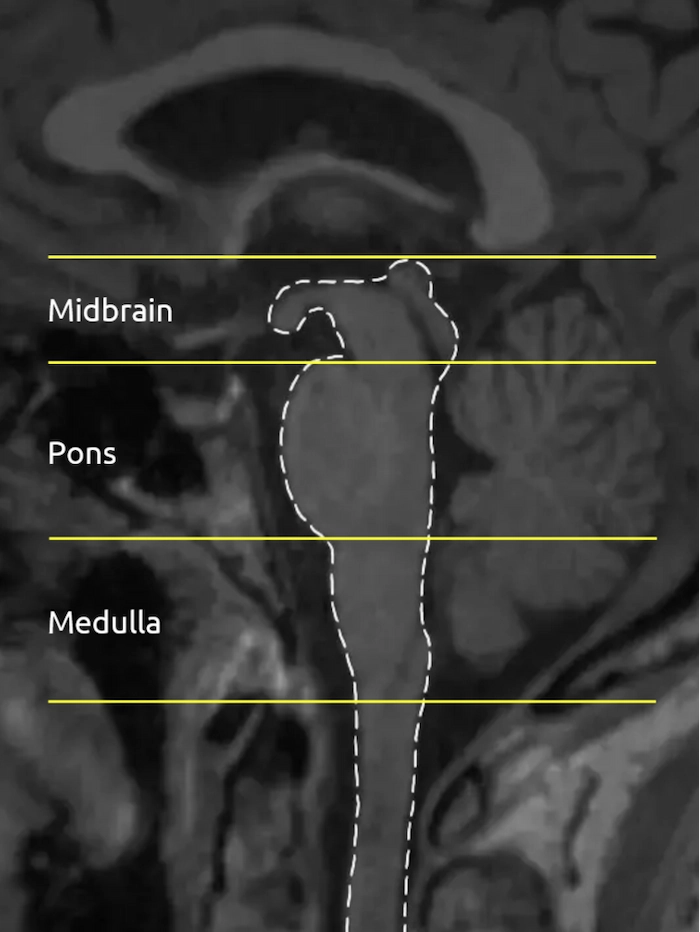
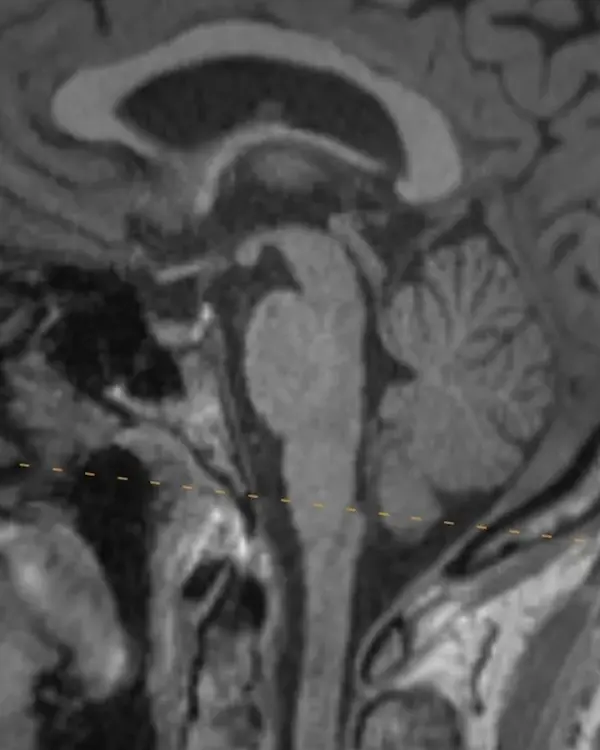
Brainstem Divisions
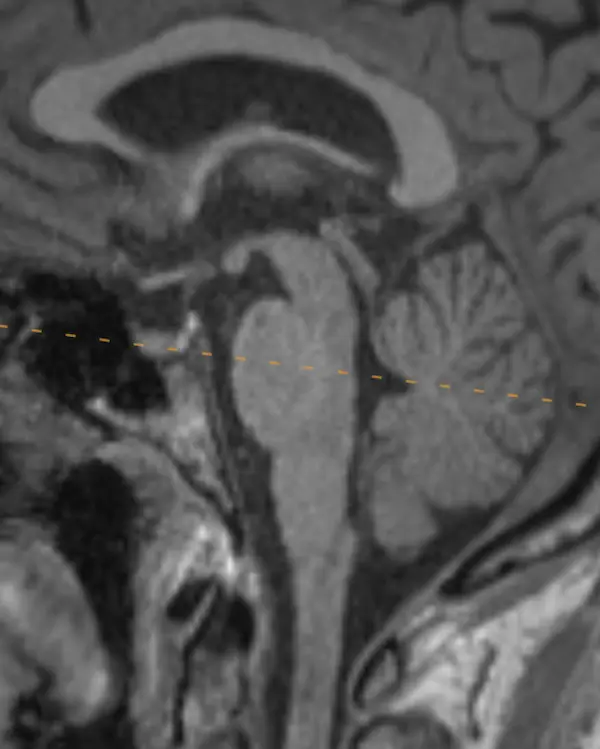
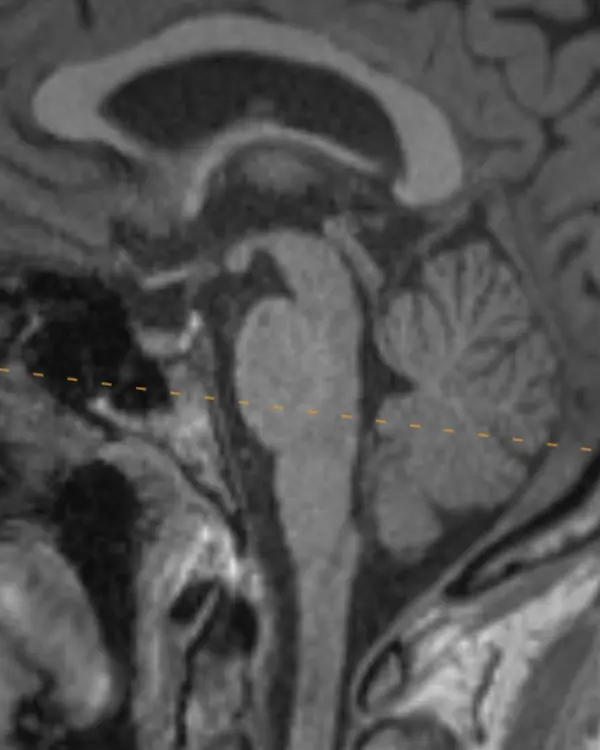
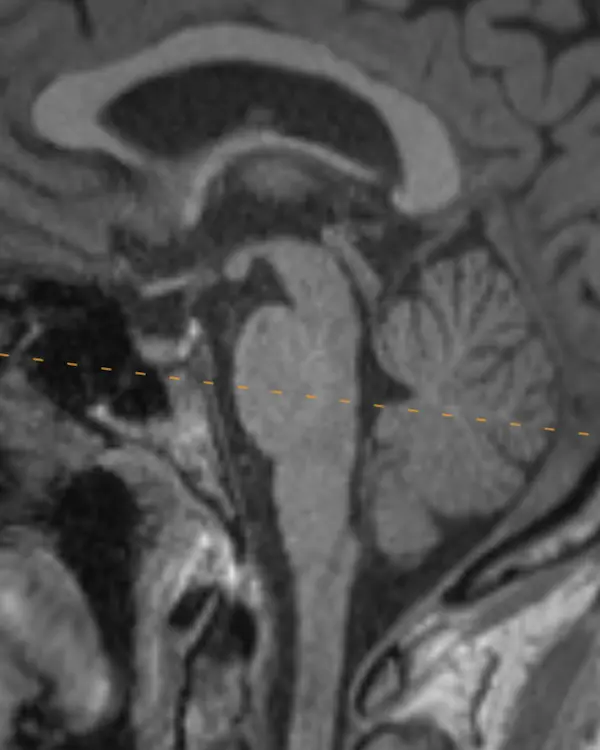
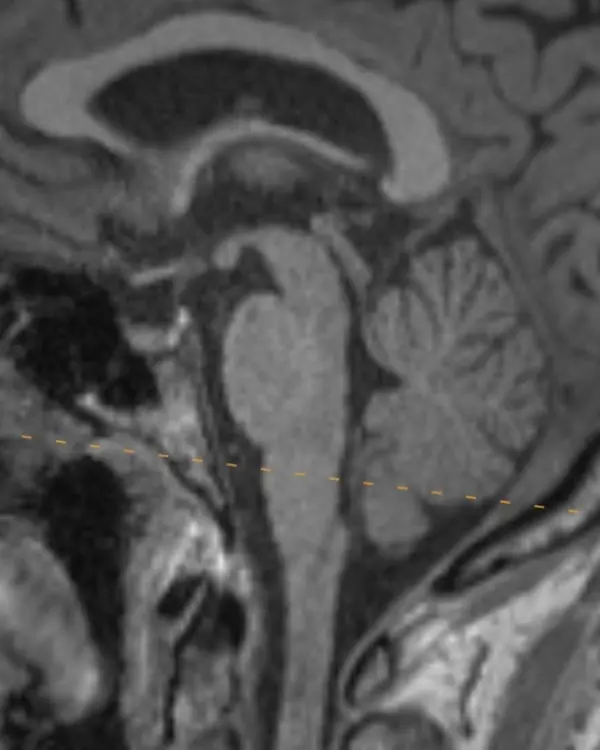
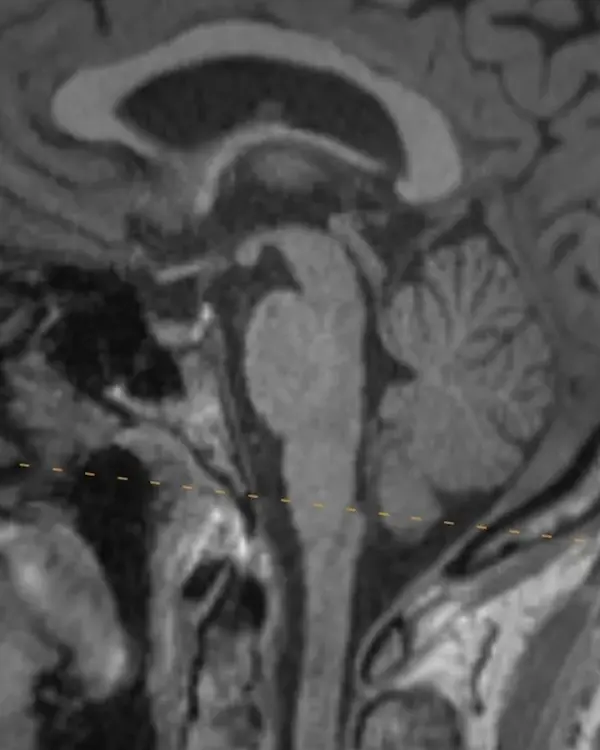
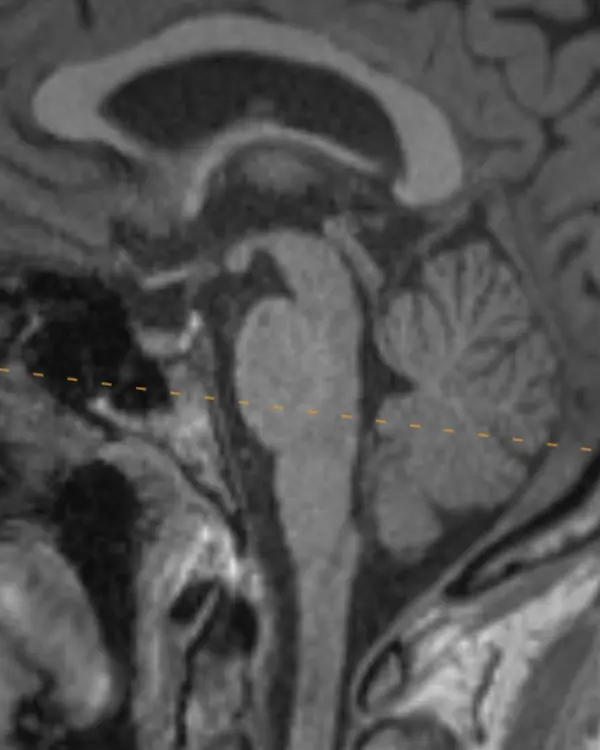
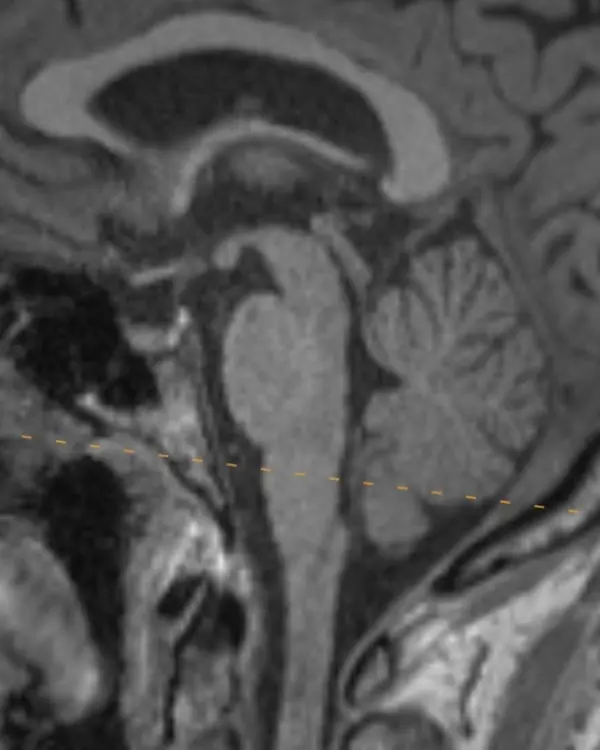
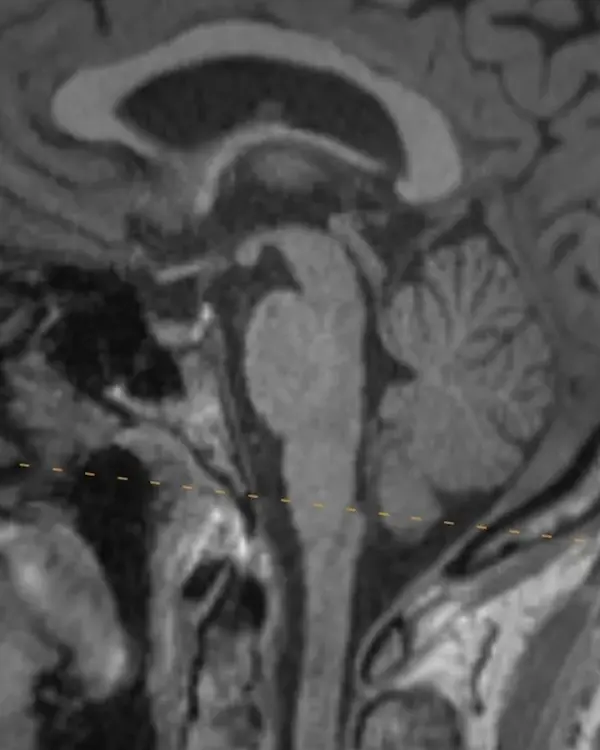
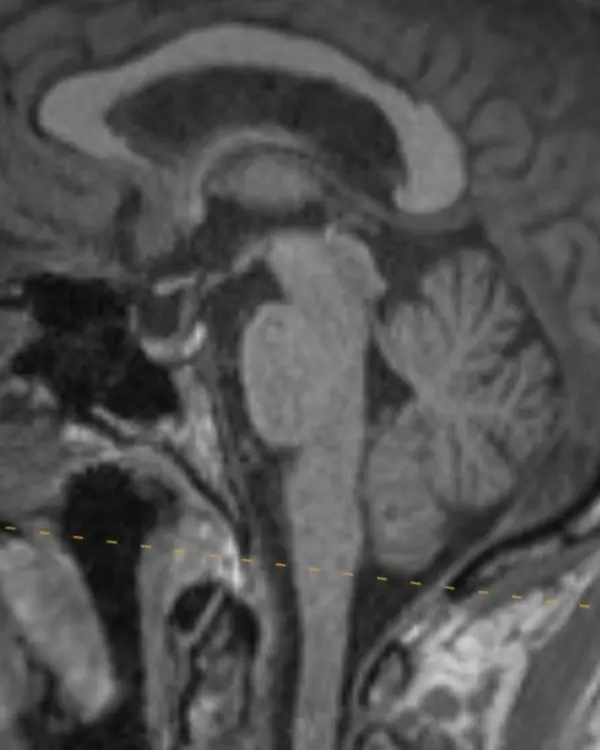
The brainstem, outlined in a white dotted line, is divided into the midbrain, pons, and medulla. Each segment has a characteristic appearance that is easiest to recognize in the sagittal plane.
Notice the beak-shaped anterior margin of the midbrain and the cerebrospinal fluid (CSF) space underneath it.
The pons has a bulbous contour anteriorly and a triangular shaped CSF space posterior to it.
The medulla is thin, gradually blends in appearance with the cervical spinal cord, and has a small CSF channel posterior to it.
Although easiest to see in the sagittal plane, these and some additional features that are unique to each division can be used to orient yourself in the axial plane.
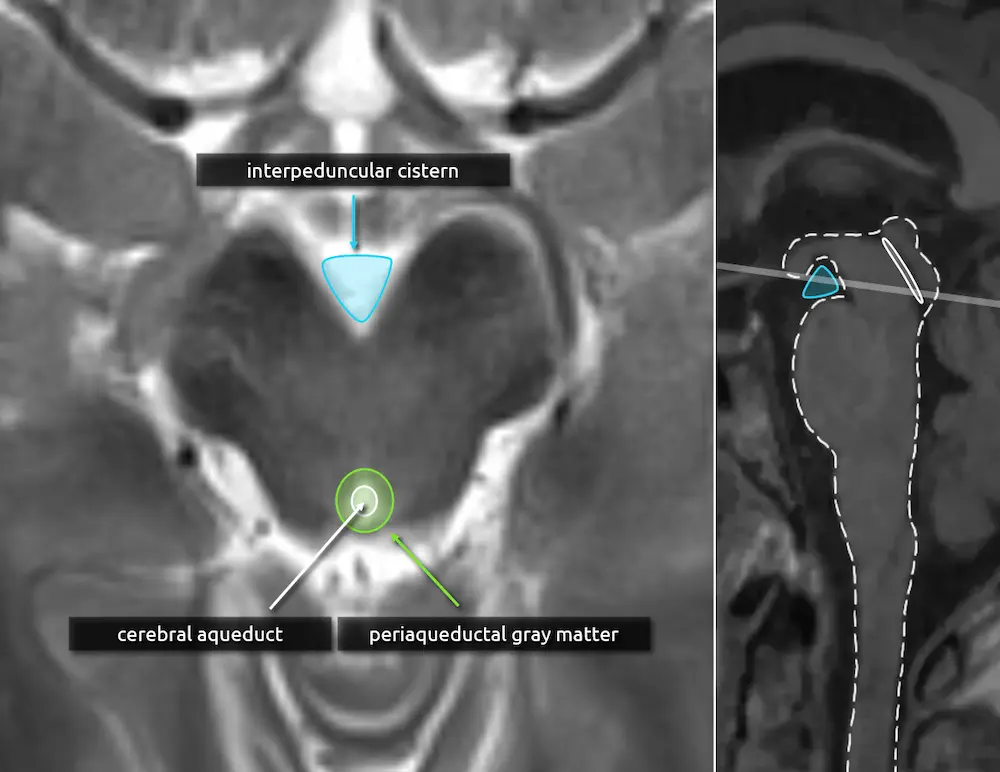
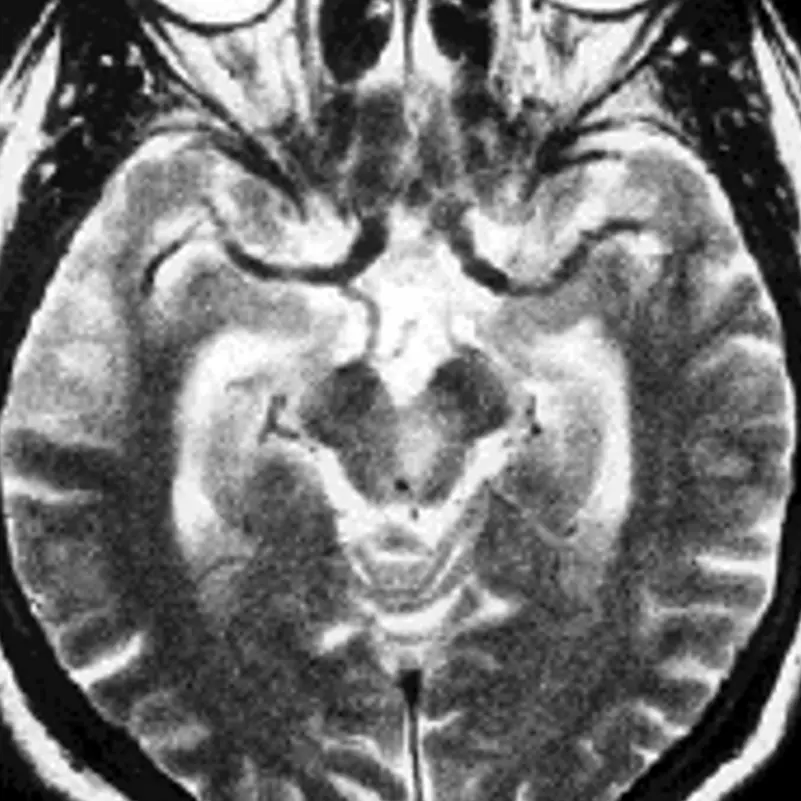
Axial Localizing Landmarks
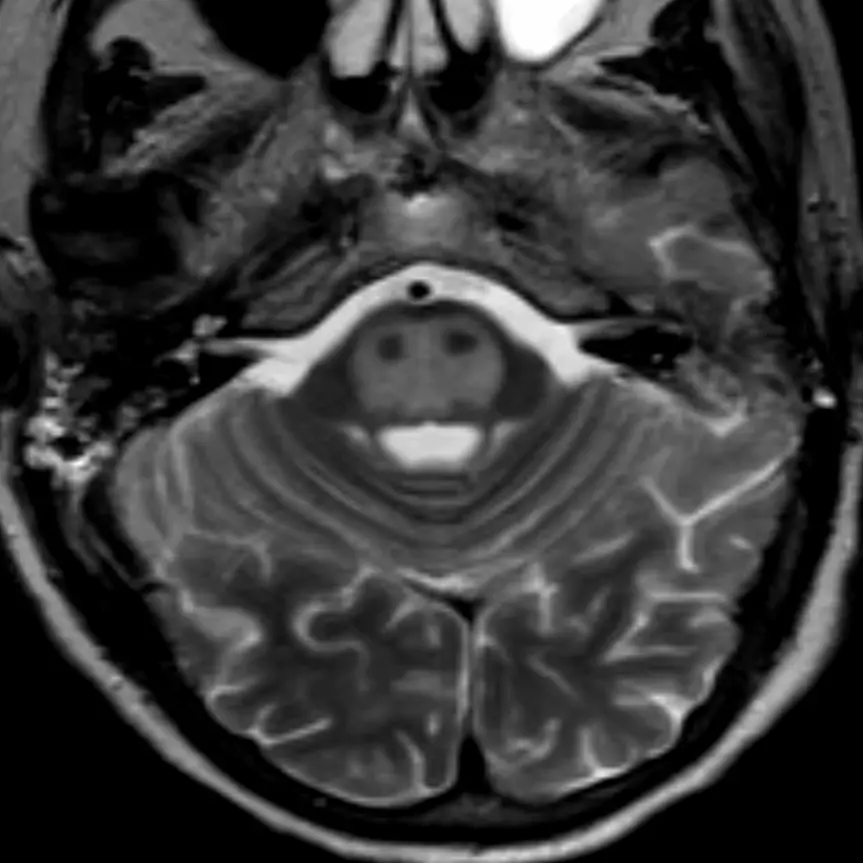
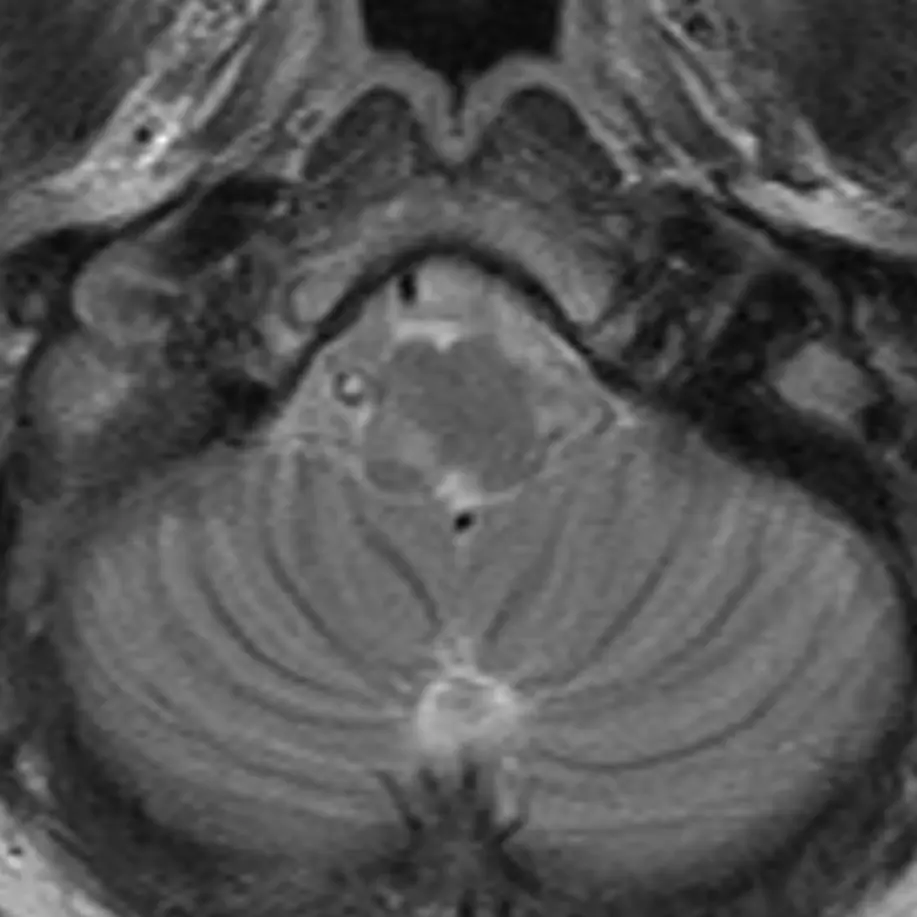
The midbrain in axial cross section has a "Mickey Mouse" appearance, most obvious in the rostral (upper) part.
1. Interpeduncular cistern
The interpeduncular cistern is the triangular CSF space located between the ears of the "Mickey Mouse." When a patient is lying flat on their back, like during a brain MRI, it is a dependent position and may collect small volume subarachnoid hemorrhage.
2. Cerebral aqueduct
The cerebral aqueduct (of Sylvius) is a thin CSF channel that courses through the midbrain, connecting the third and fourth ventricles. Stenosis of the cerebral aqueduct is the most common cause of congenital hydrocephalus.
3. Periaqueductal gray matter (see below)

Midbrain
Rostral
1. Interpeduncular cistern
2. Cerebral aqueduct
The caudal (lower) midbrain loses the eyes of the "Mickey Mouse," which correspond to the red nuclei (see level 3).
3. Periaqueductal gray matter
The periaqueductal gray matter is a rim of gray matter surrounding the cerebral aqueduct. Abnormal signal intensity here is common and nonspecific but classically is a feature of Wernicke encephalopathy.
Midbrain
Caudal
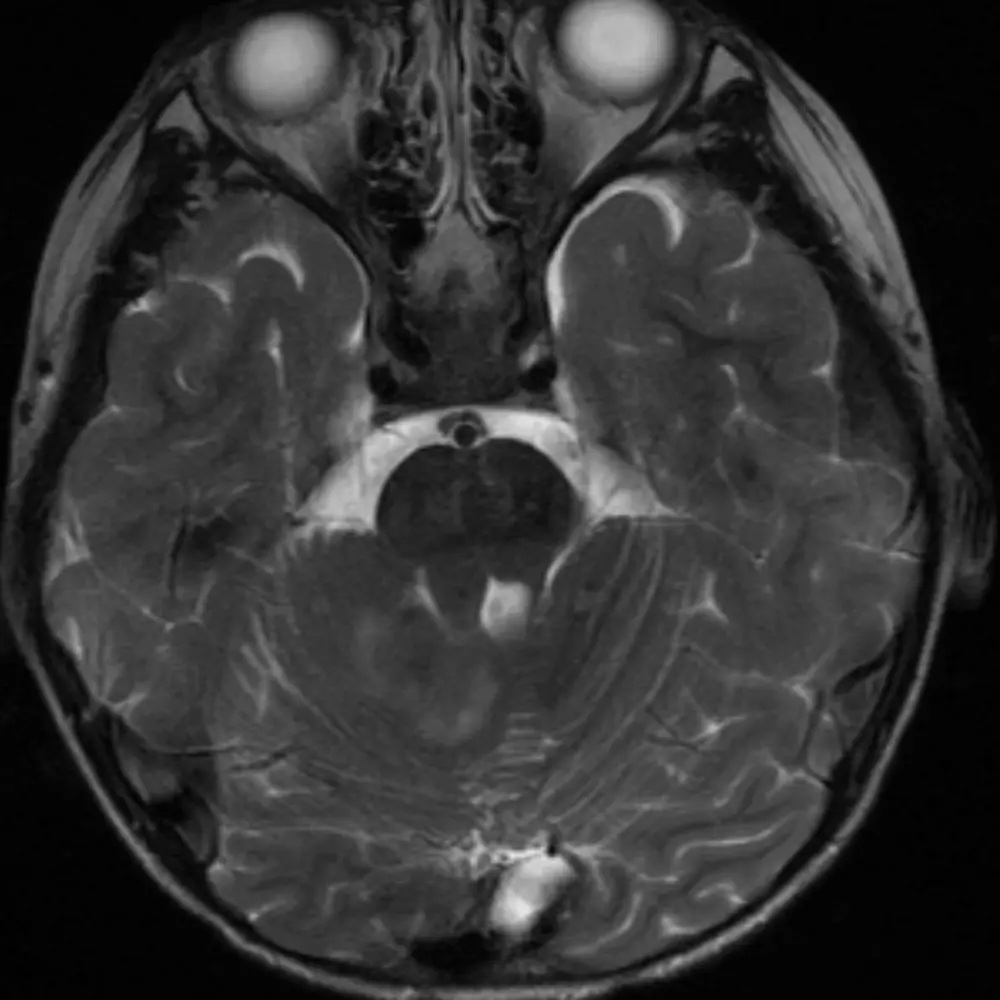
The pons' bulbous contour in the sagittal plane can also be seen on axial cuts. The "Mickey Mouse" appearance of the midbrain is no longer visible.
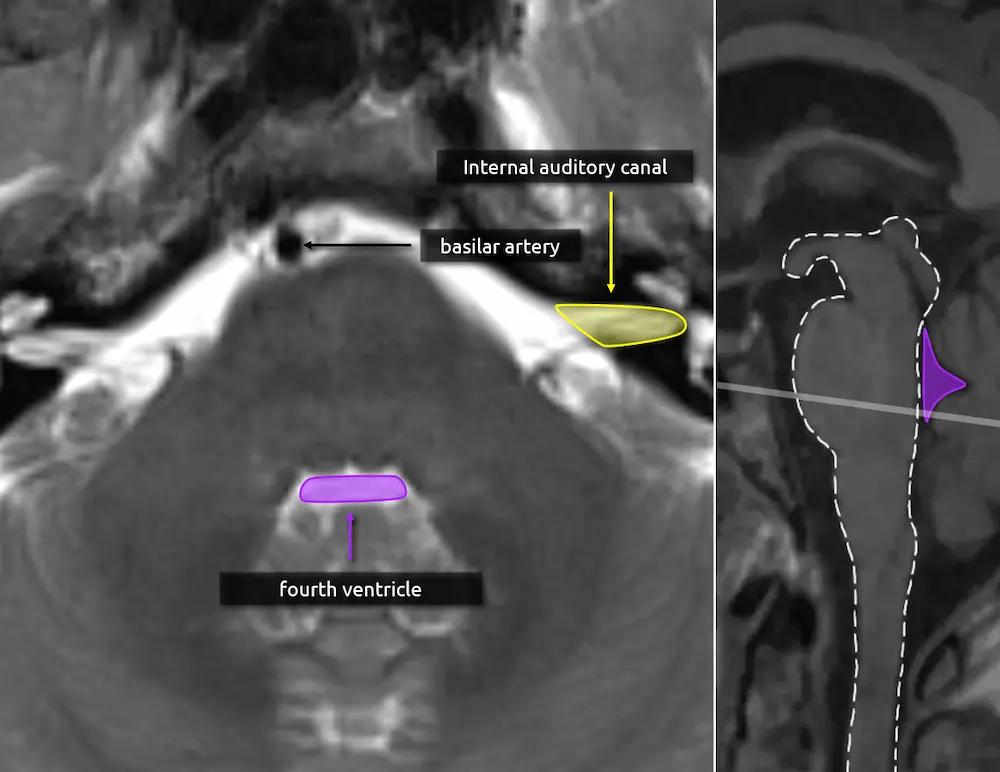
1. Fourth ventricle
The triangular CSF space posterior to the pons is the fourth ventricle. It should be seen on every head CT or brain MRI and, if it is not, there is likely pathology. Effacement of the fourth ventricle may be an early sign of mass effect, either due to a lesion or edema.
2. Basilar artery
The basilar artery courses along the surface of the pons. It should always be dark on a T2-weighted image. A bright basilar artery is a sign that blood has stopped moving or is moving slowly (i.e. "loss of flow void"), suggesting an occlusion.
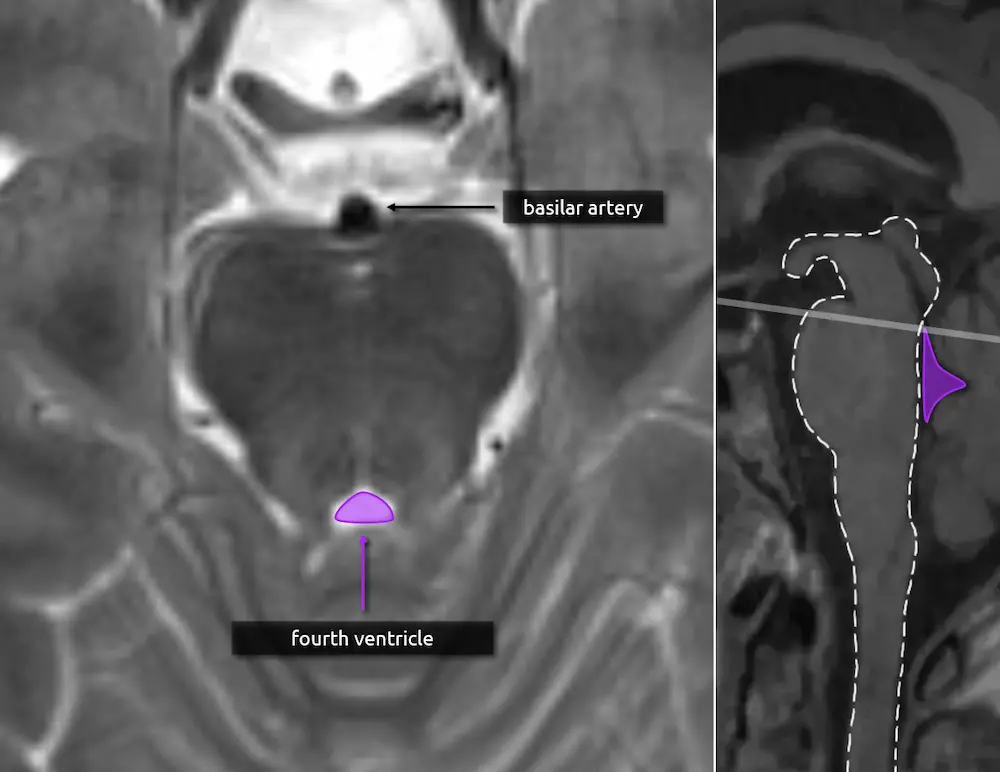
Pons
Rostral
1. Fourth ventricle
2. Basilar artery
View the images on the right to see how the caliber of the fourth ventricle changes as you scroll up and down. The fourth ventricle's caliber is largest at the mid aspect of the pons.
1. Fourth ventricle
2. Basilar artery
3. Internal auditory canal
The internal auditory canals (IACs) are useful landmarks to identify the caudal (lower) part of the pons and thus several important nuclei that will be introduced in later levels.
Pons
Caudal
The lateral borders of the medulla are concave compared to the bulbous, convex borders of the pons.
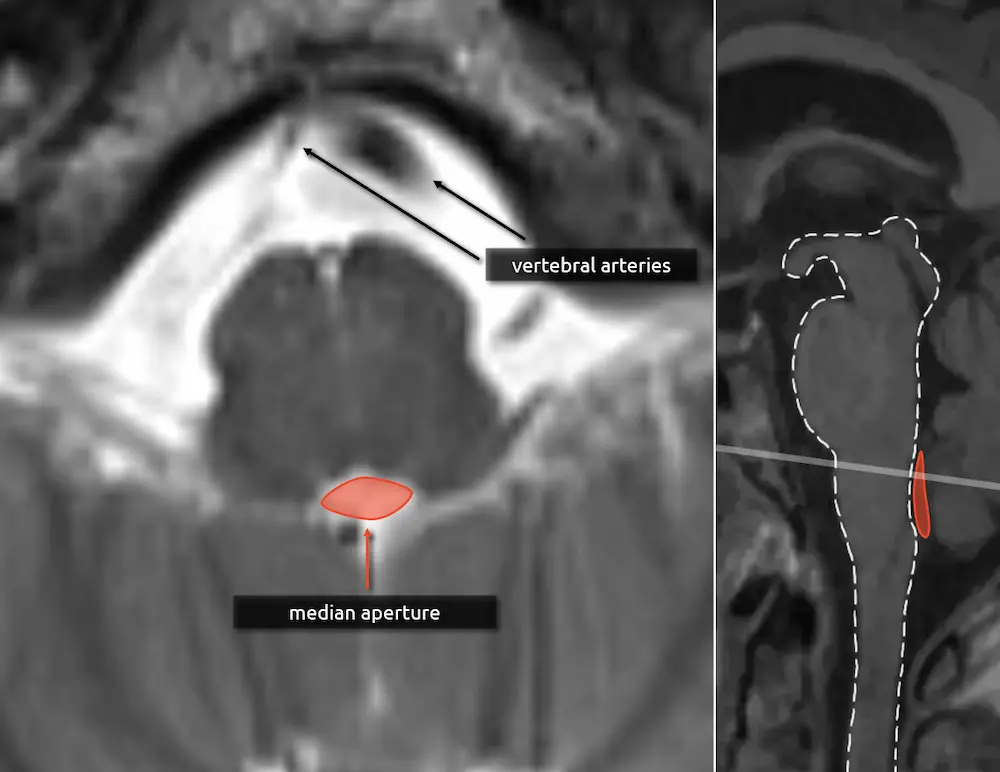
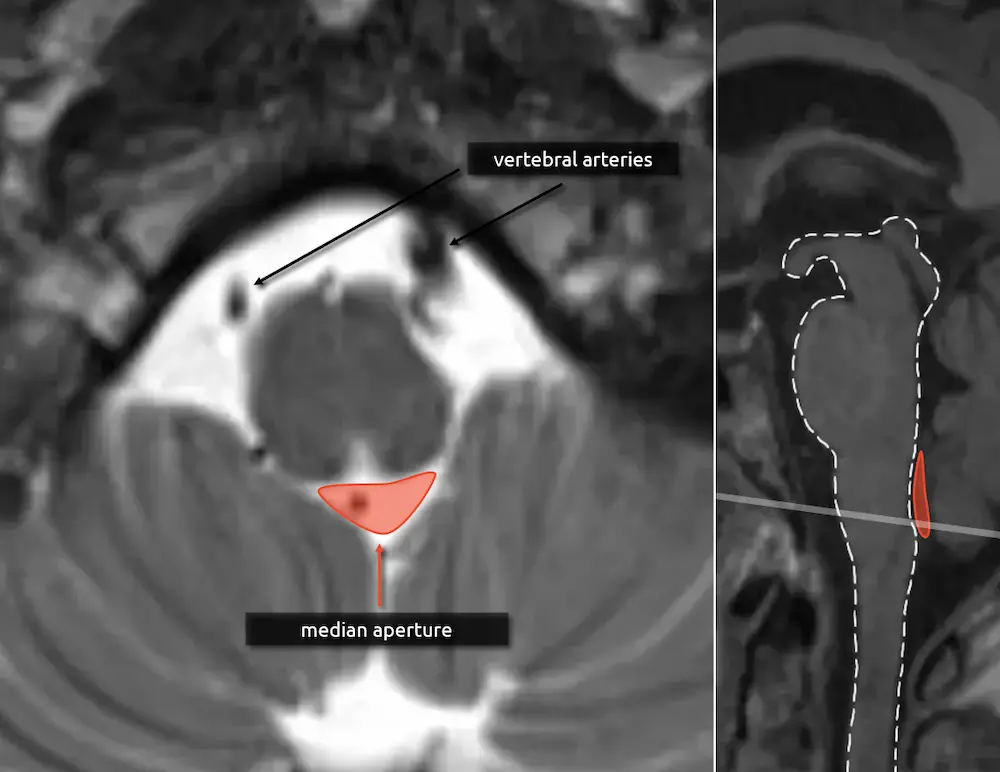
1. Median aperture
The median aperture, or the foramen of Magendie, is the thin CSF space posterior to the medulla and medial drainage pathway of the fourth ventricle. There are two more holes in the lateral aspect of the fourth ventricle, called the lateral apertures or foramina of Luschka. Together, these are the three ways that CSF can flow inferiorly into the cisterna magna.
2. Vertebral arteries
The vertebral arteries fuse to form the basilar artery approximately at the level of the upper medulla. If they are present, then you are likely at the level of the medulla in the absence of variant anatomy (e.g. basilar nonfusion).
Medulla
Rostral
1. Median aperture
2. Vertebral arteries
The medulla gradually transitions to the shape of the cervical spinal cord. The median aperture does not significantly change along its course.
Medulla
Mid
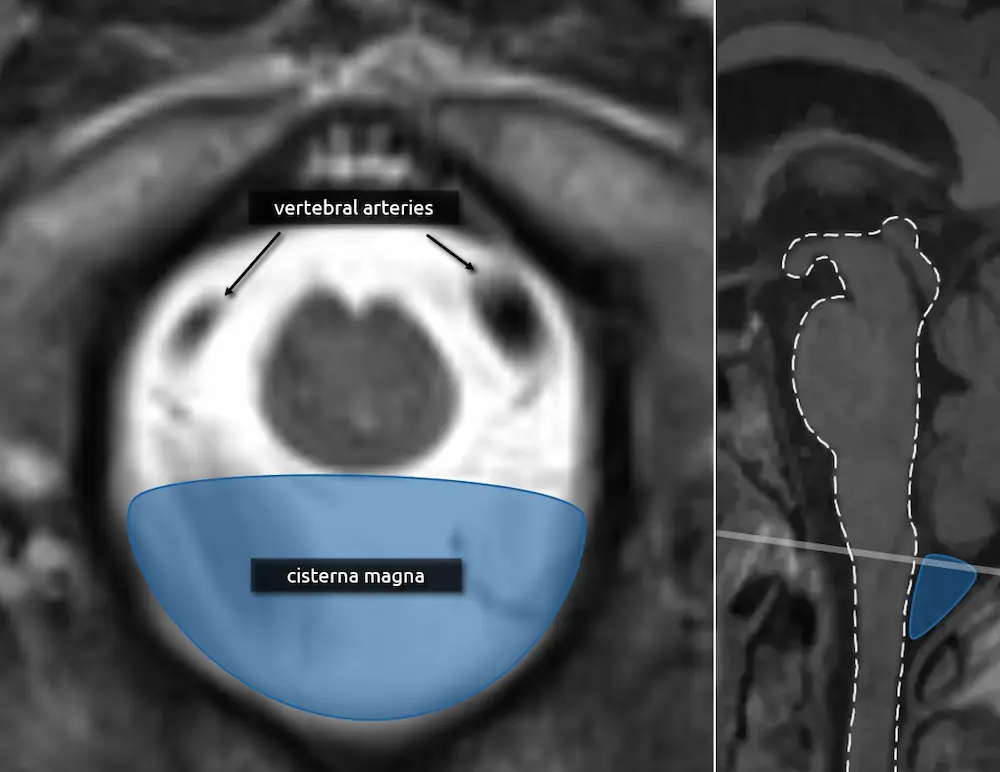
The transition of the medulla to the cervical spinal cord is approximated by the foramen magnum. At this point, the medulla is nearly completely round.
1. Vertebral arteries
2. Cisterna magna
The cisterna magna is the largest CSF space in the brain and is located posterior to the lower medulla/cervicomedullary junction. The CSF space lateral to the medulla is called the lateral cerebellomedullary cistern, and the CSF space anterior to the medulla is the premedullary cistern.
Medulla
Caudal
Level 2
Midbrain
- Cerebral peduncles
- Superior colliculi
- Inferior colliculi
- Decussation of the superior cerebellar peduncles
Pons
- Decussation of the superior cerebellar peduncles (continued)
- Superior cerebellar peduncles
- Corticospinal tracts
- Middle cerebellar peduncles
- Transverse pontine fibers
Medulla
- Pyramids
- Inferior cerebellar peduncles
- Spinocerebellar tracts
- Pyramidal decussation
Introduction to Sectional Anatomy
The internal anatomy of the brainstem is extremely dense. Many of the important internal structures are not identifiable on routine imaging and their location may only be approximated using landmarks. Level 2 will introduce some of the more salient and useful landmarks crucial for inferring the location of other structures in the proceeding complexity levels.
Note that axial planes in brain imaging are not perfectly perpendicular to the brainstem, they are instead created by drawing a line through the anterior commissure (AC) and posterior commissure (PC); the so-called AC-PC line. Keep this in mind when correlating the appearance of structures in the axial plane to sagittal.
Rostral
Midbrain
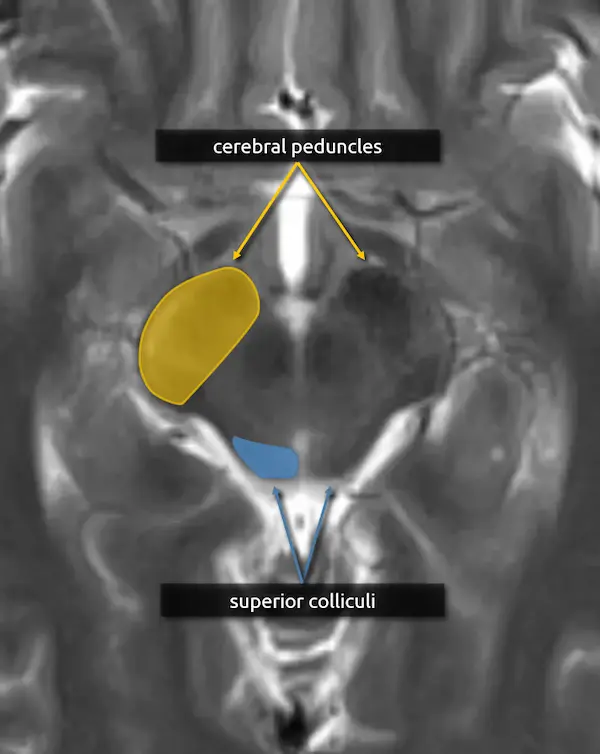
1. Cerebral peduncles:
The cerebral peduncles are located in the ventral midbrain and connect the midbrain to the cerebrum. They contain large named white matter tracts that are important for motor function, for example:
a. Corticospinal tract (limbs and trunk)
b. Corticobulbar tract (face and neck)
c. Corticopontocerebellar tract (coordination)
The individual tracts are not well visualized on routine imaging, but the corticospinal tract is the largest and is roughly in the center of the peduncle; see level 5 for more detail.
Mass effect of the cerebral peduncle is an important sign of uncal herniation.
2. Superior colliculi:
The superior colliculi are located in the caudal midbrain along the dorsal aspect, forming two of the four bumps on the surface. They are important for coordinating eye movements towards motion and visual stimuli. There are white matter tracts connecting the superior colliculi to areas crucial for coordinated motor function, such as the basal ganglia and substantia nigra (see level 3).
Atrophy of the superior colliculi in progressive supranuclear palsy contributes to the characteristic vertical gaze palsy.

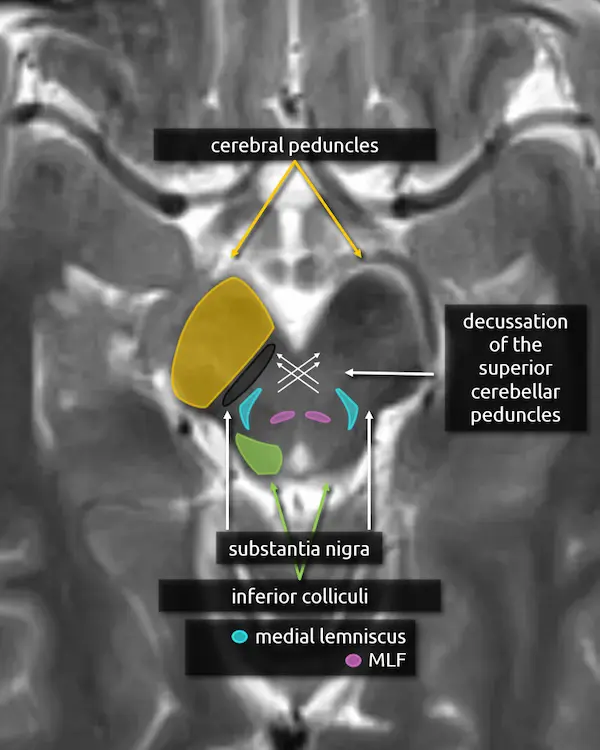
Caudal
Midbrain
1. Cerebral peduncles
2. Inferior colliculi
The inferior colliculi are located a slice below the superior colliculi and form two more bumps along the caudal aspect of the dorsal midbrain. They are important in perception and integration of auditory stimuli. The inferior border of the inferior colliculi is used as a marker for the transition from midbrain to pons.
The superior and inferior colliculi may be referred to collectively as the quadrigeminal plate or the tectum (see level 5).
3. Decussation of the superior cerebellar peduncles
The superior cerebellar peduncles are seen in the next section, but they cross at this level in the center of the midbrain as the fibers travel superiorly.
The fibers of the superior cerebellar peduncles are highly organized causing water molecules to move along the myelin sheaths in relatively uniform directions (i.e. anisotropy). This often causes mild physiologic diffusion restriction that may be misinterpreted as an infarction. Nonetheless, infarction in this region can occur characterized by bilateral cerebellar ataxia called Wernekinck commissure syndrome, which is highly unlikely without supporting clinical history. Absence of this decussation occurs in Joubert syndrome and other ciliopathies, producing a "molar tooth" appearance of the midbrain.


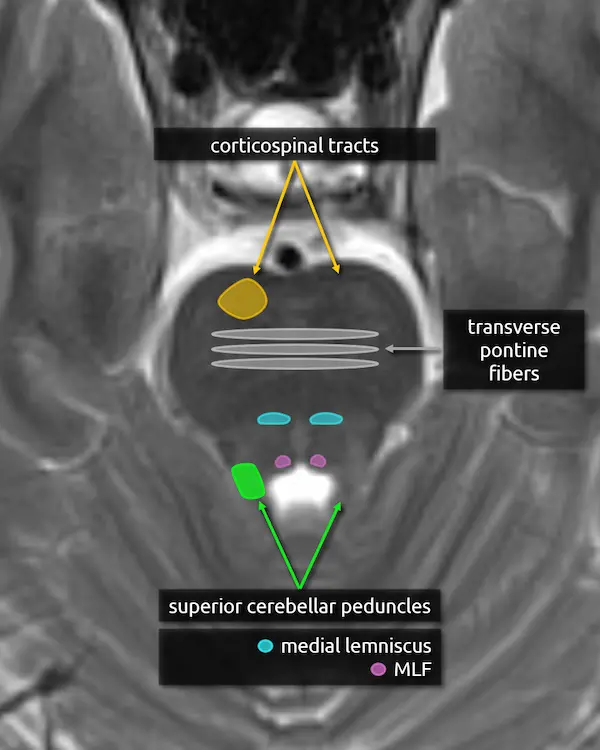
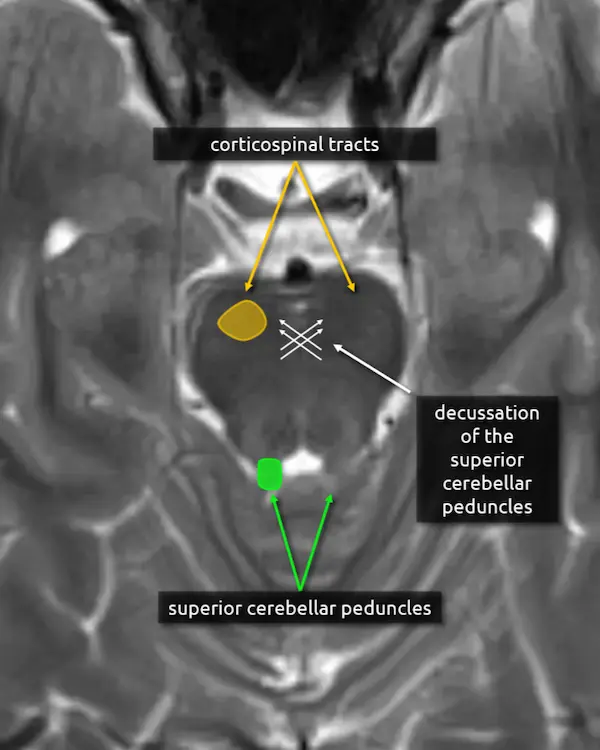
Rostral
Pons
1. Decussation of the superior cerebellar peduncles
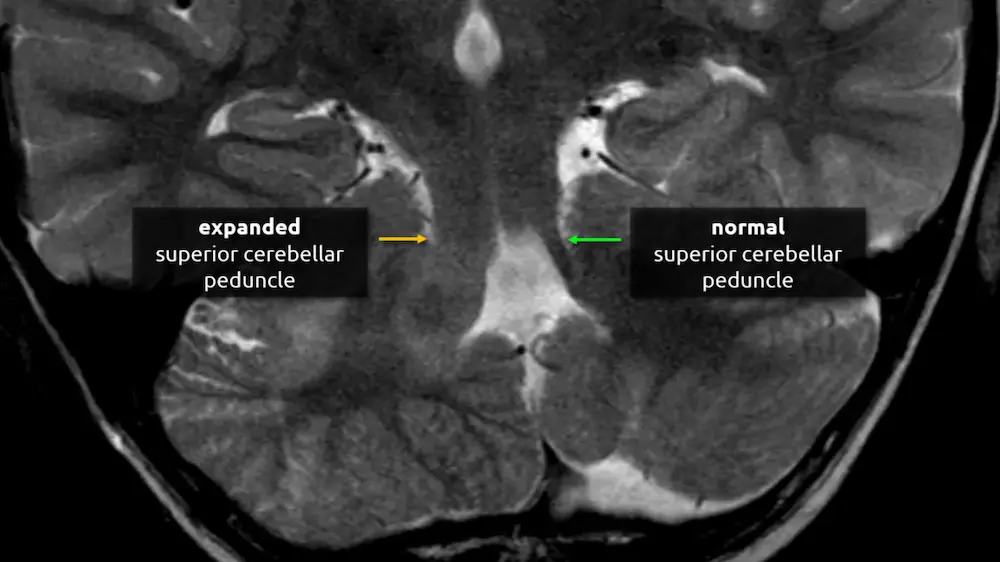
2. Superior cerebellar peduncles
The superior cerebellar peduncles are the most superior of the three paired white matter bundles that connect the cerebellum to the brainstem. Their fibers are mostly efferent, beginning at the dentate and emboliform nuclei of the cerebellum and terminating at the contralateral thalamus and the red nucleus, located in the upper midbrain (see level 3).
Atrophy of the superior cerebellar peduncles can be seen in several conditions, such as progressive supranuclear palsy and other Parkinsonian disorders.
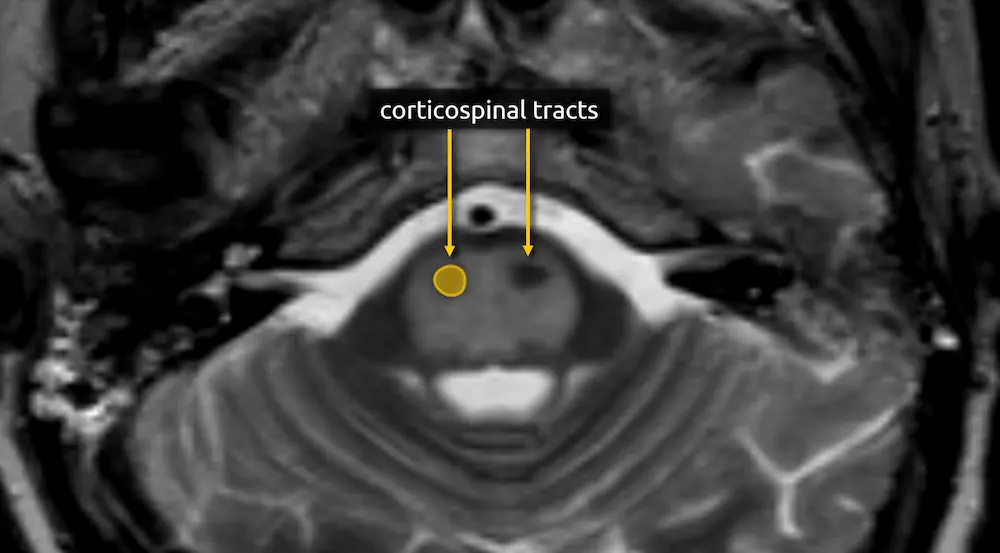
3. Corticospinal tracts
The corticospinal, corticobulbar, and corticopontocerebellar tracts continue inferiorly from the cerebral peduncles.
Lesions of the corticospinal tracts will cause motor deficits of the body and limbs. Sparing or involvement of the corticospinal tracts is a characteristic finding of several conditions, e.g., sparing of the corticospinal tracts is responsible for the "trident sign" of osmotic demyelination syndrome. The corticobulbar tract is located along the medial aspect and can be selectively damaged at this level, producing facial weakness.

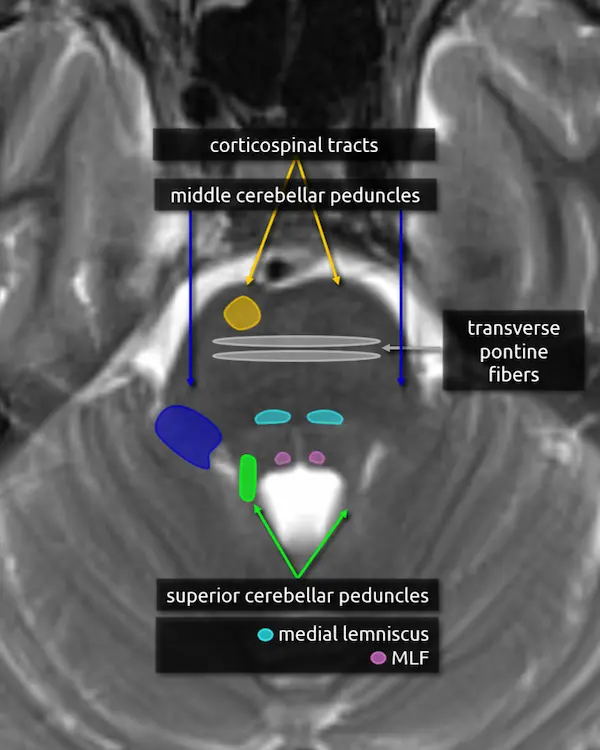
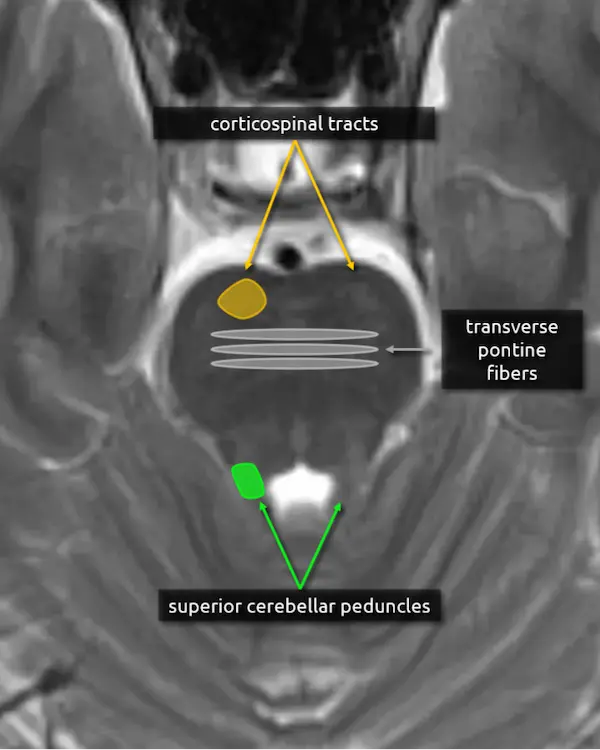
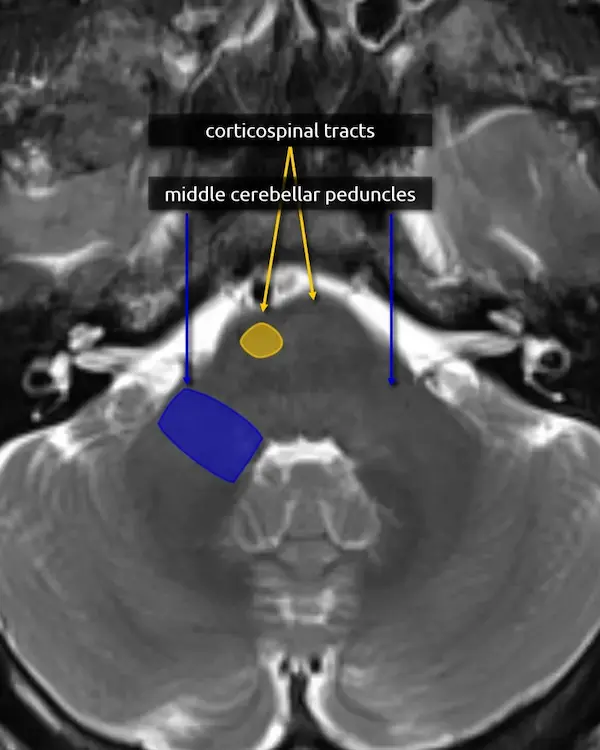
Mid
Pons
1. Corticospinal tracts
2. Superior cerebellar peduncles
3. Middle cerebellar peduncles:
The middle cerebellar peduncles are the largest of the cerebellar peduncles and connect the cerebellum to the pons. The fibers are entirely afferent, originating from contralateral pontine nuclei and terminating in the cerebellum. Over 90% of the fibers in the middle cerebellar peduncles belong to the corticopontocerebellar pathway (see below).
There are many causes of middle cerebellar peduncle signal abnormality, usually resulting from conditions that can cause white matter edema, degeneration, or gliosis. Bilateral T2 hyperintensity of the middle cerebellar peduncles is a classic but not specific sign of fragile X-associated tremor/ataxia syndrome (FXTAS). Multiple system atrophy cerebellar type (MSA-C) and spinocerebellar ataxia are other classic causes of middle cerebellar peduncle atrophy and signal abnormalities.
4. Transverse pontine fibers:
The transverse pontine fibers form the bulk of the mid pons and are crossing white matter tracts that go to, or come from, the cerebellum via the middle cerebellar peduncles. The majority of the fibers belong to the corticopontocerebellar pathway, which is crucial for motor coordination and learning.
A lesion that involves the transverse pontine fibers is likely to produce ataxia.

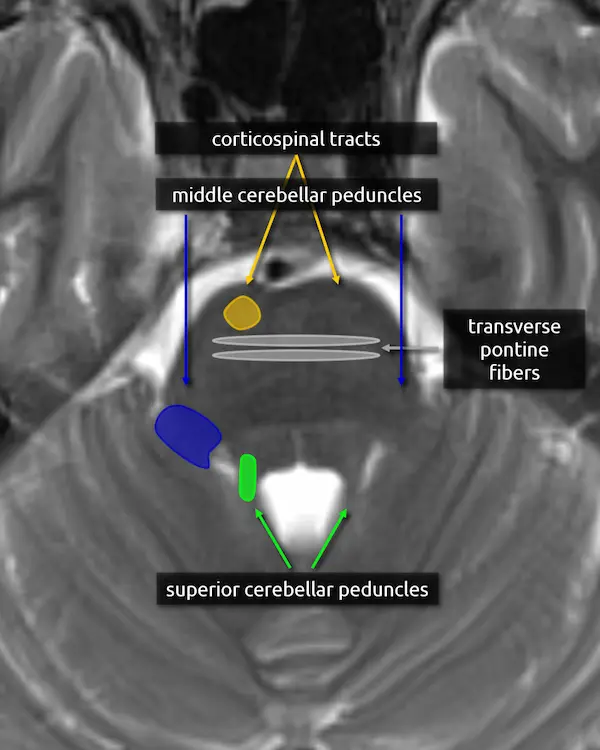
Caudal
Pons
1. Corticospinal tracts
2. Middle cerebellar peduncles
No new structures are introduced at this level.
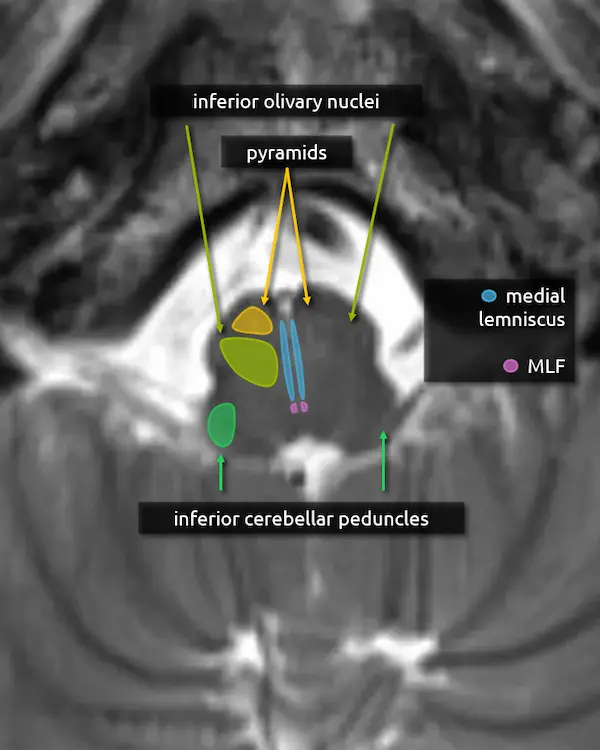
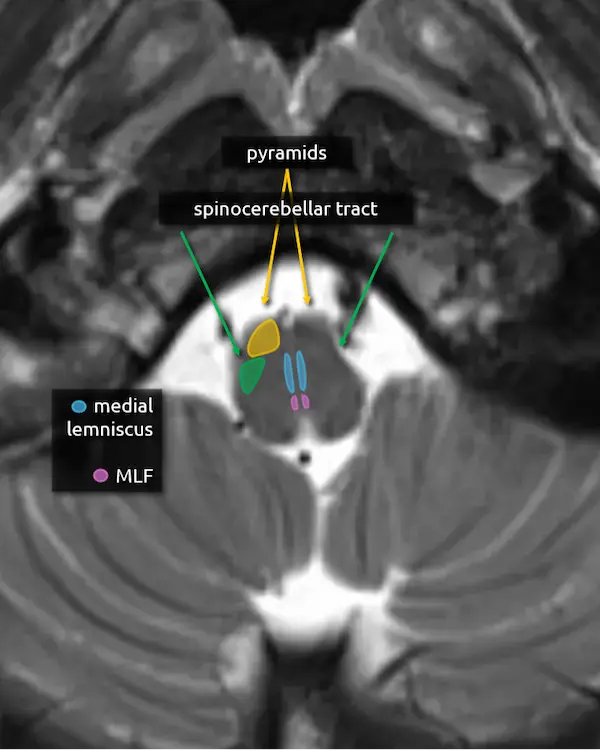
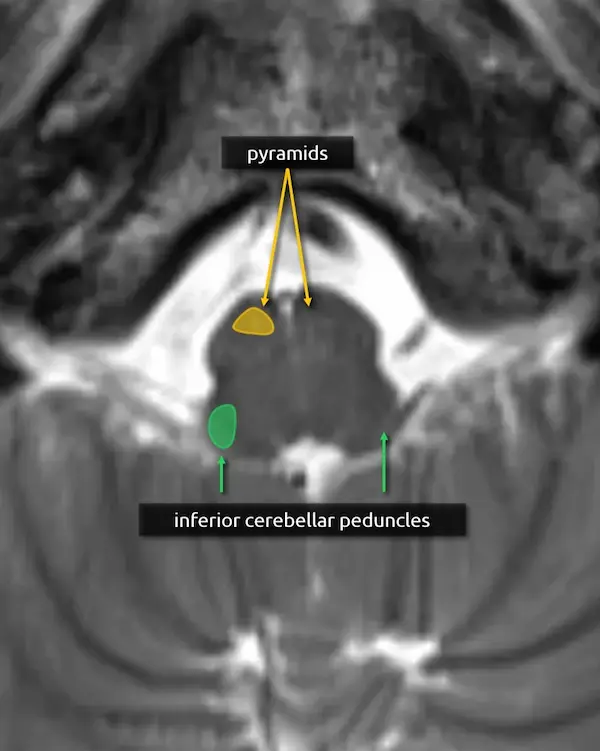
Rostral
Medulla
1. Pyramids:
The medullary pyramids contain the corticospinal tract and corticobulbar tract, which are sometimes collectively called the pyramidal tracts. They are named due to the shape they form on the ventral surface of the medulla, which usually becomes more pyramid-like inferiorly.
2. Inferior cerebellar peduncles:
The inferior cerebellar peduncles are the smallest of the three, making them difficult to recognize in the axial plane. They contain mostly afferent and few efferent fibers.
Hyperintensity of the inferior cerebellar peduncle has recently been proposed as a specific feature of multiple system atrophy cerebellar type (MSA-C), helping differentiate it from spinocerebellar ataxia (inferior cerebellar peduncle sign).
Mid
Medulla
1. Pyramids
2. Spinocerebellar tracts:
The spinocerebellar tracts are ascending tracts from the spinal cord to the cerebellum involved in proprioception of the trunk and lower limbs. They are separated into ventral and dorsal divisions; the dorsal division travels to the cerebellum via the inferior cerebellar peduncle and the anterior division goes through the superior cerebellar peduncle. To reach the superior cerebellar peduncle, the anterior spinocerebellar tract travels along the lateral margin of the corticospinal tract through the pons. The spinocerebellar tract is best approximated posterior to the pyramids in the mid to lower medulla, where the ventral and dorsal division remain together.
The upper limb equivalent of the spinocerebellar tract is the cuneocerebellar tract, which is smaller and located medially.
Lesions involving these tracts will cause ataxia.
.webp)
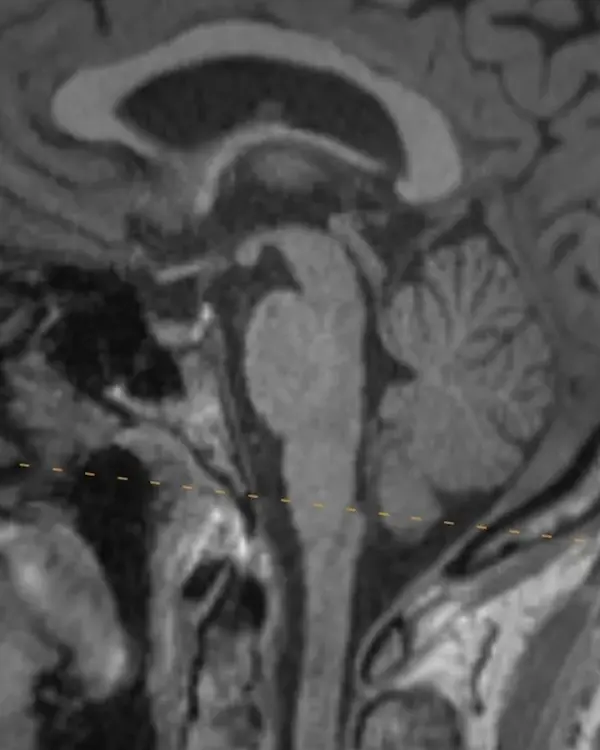
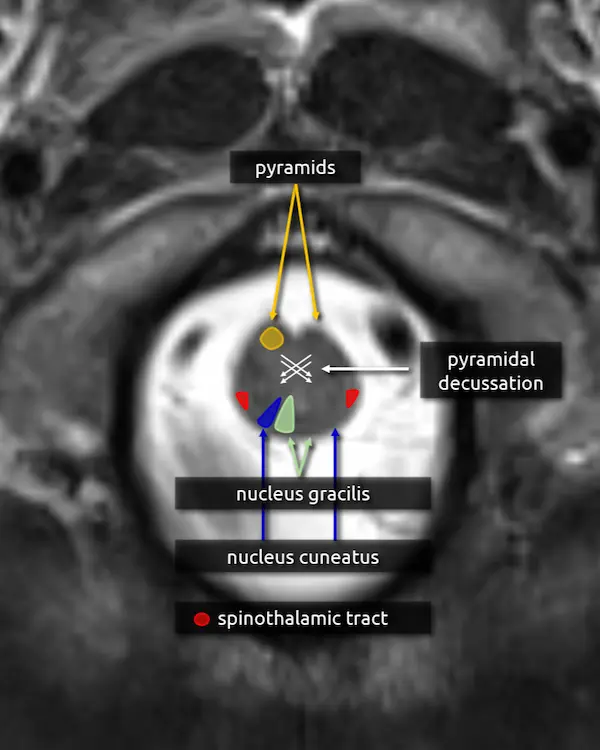
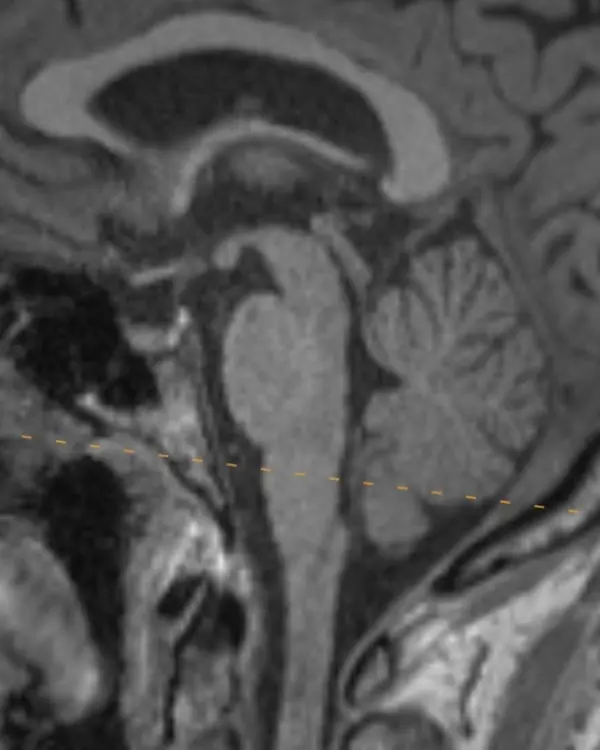
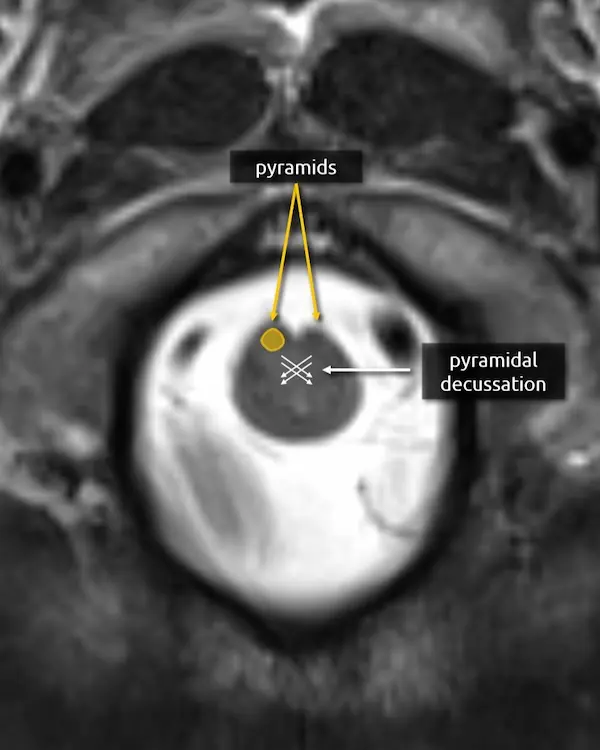
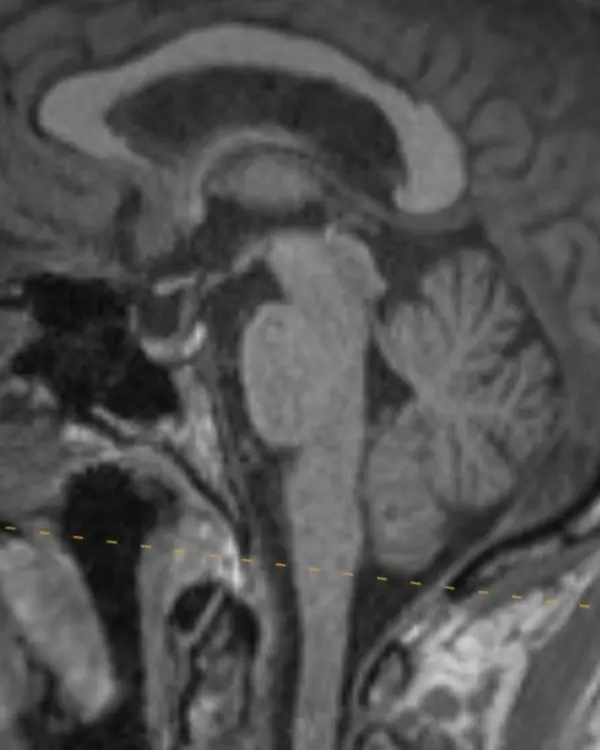
Caudal
Medulla
1. Pyramids
2. Pyramidal decussation:
The medulla transitions to the cervical spinal cord at about the level of the craniocervical junction. Right before this transition, about 90% of the corticospinal tract fibers traveling through the pyramids cross the pyramidal decussation before continuing through the spinal cord as the lateral corticospinal tract. The other 10% form the anterior corticospinal tract. On cross-sectional imaging, the approximate location of the decussation is inferred using the skull base and foramen magnum as landmarks.
Question 1
a. What structure is the abnormality centered within?


Question 2
a. What tract is spared by the abnormality?

Practice Questions
Level 2
Question 3
A 8-year-old boy presents with difficulty walking.
a. What brainstem structure is asymmetrically enlarged?

Level 3
Midbrain
- Red nucleus
- Substantia nigra
- Medial lemniscus
- Medial longitudinal fasciculus (MLF)
Pons
- Medial lemniscus (continued)
- Medial longitudinal fasciculus (MLF) (continued)
- Trigeminal (CN V) nerve root
- Trigeminal (CN V) main sensory nucleus
- Trigeminal (CN V) motor nucleus
Medulla
- Medial lemniscus (continued)
- Medial longitudinal fasciculus (MLF) (continued)
- Inferior olivary nucleus
Rostral
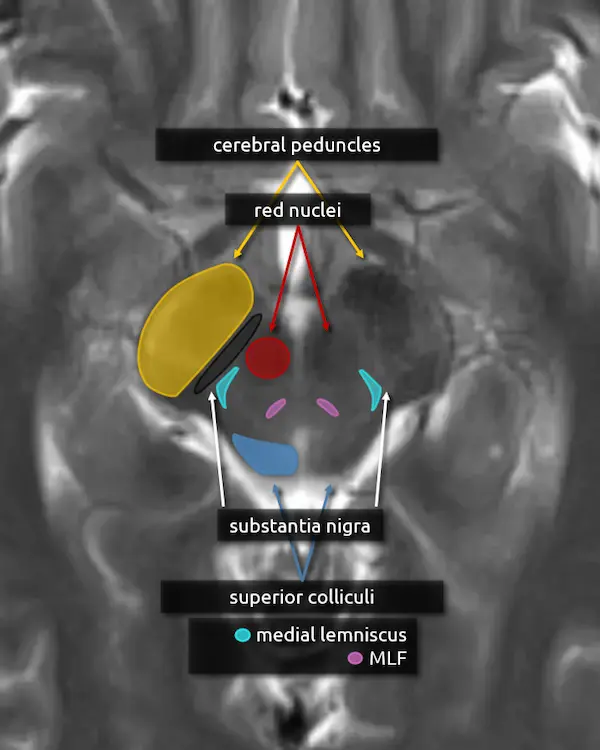
Midbrain
1. Cerebral peduncles
2. Superior colliculi
3. Red nucleus
The red nucleus is a component of the extrapyramidal motor system. It takes input from the cerebellum (via the superior cerebellar peduncles), motor, premotor, and frontal cortices and projects to the contralateral cervical spinal cord and, to a lesser extent, the ipsilateral inferior olivary nucleus (see rostral medulla below) via the rubrospinal tract. The red nuclei are dark on T2-weighted MRI images, producing the eyes of the "Mickey Mouse" appearance of the upper midbrain.
Focal damage to the red nucleus is rare but may occur in paramedian midbrain syndrome (Benedikt syndrome). Lesions in this region characteristically cause contralateral tremor, ataxia, and involuntary limb movements (choreoathetosis). The red nucleus is also used as a border for the localization of posturing; decerebrate posturing usually results from lesions at or below the red nucleus and decorticate posturing from lesions above.
4. Substantia nigra
The substantia nigra is a large nucleus at the base of the cerebral peduncle that spans the midbrain. It is a major component of the extrapyramidal motor system and has bidirectional connections between the striatum (caudate and putamen), forming the nigrostriatal pathway. It is composed of two areas: the pars compacta and the pars reticulata.
Loss of dopamine producing neurons in the pars compacta is a defining feature of Parkinson's disease.
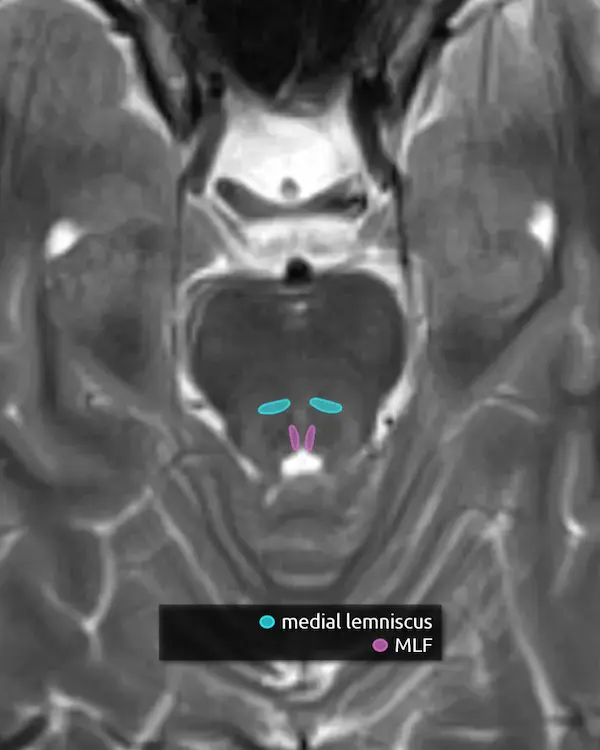
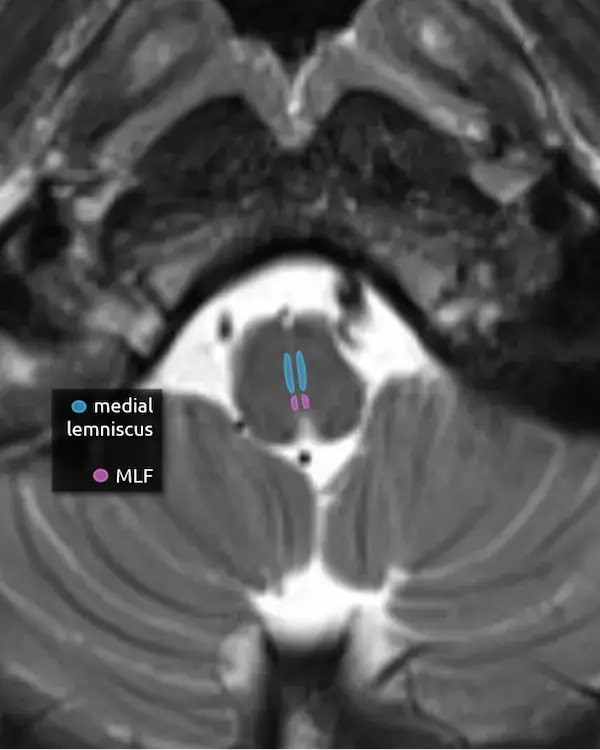
5. Medial lemniscus
The medial lemniscus is an ascending sensory pathway that spans the entire brainstem, originating at the nucleus gracilis and cuneatus (see level 5) in the medulla and ending at the primary sensory nucleus of the thalamus: the ventral posterolateral nucleus (VPL). It begins medially in the medulla and becomes more lateral at the level of the midbrain, located in close proximity to the substantia nigra. It is responsible for vibration sensation, fine touch, and proprioception.
Lesions involving the medial lemniscus may cause contralateral loss of vibration sensation and joint position sensation on physical exam with symptoms of numbness and paresthesias.
6. Medial longitudinal fasciculus (MLF)
The MLF is an ascending and descending pathway responsible for coordinating eye movements. It connects all of the cranial nerve nuclei that innervate the extraocular muscles (CN III, IV, and VI) as well as the vestibulocochlear nuclei (CN VIII). The MLF spans the entire brainstem, however lesions producing visual symptoms will probably be in the midbrain or pons.
There are characteristic syndromes that result from damage to the MLF, most commonly internuclear ophthalmoplegia (INO) or INO-plus syndromes. A common clinical scenario is a patient with multiple sclerosis who develops a demyelinating lesion along the MLF in the midbrain or pons and presents with bilateral INO.
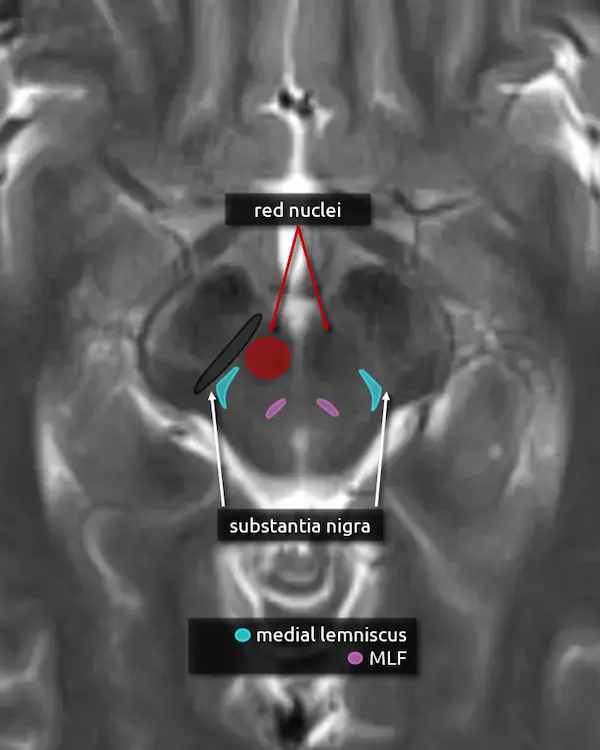

Caudal
Midbrain
1. Cerebral peduncles
2. Inferior colliculi
3. Decussation of the superior cerebellar peduncles
4. Substantia nigra
5. Medial lemniscus
6. Medial longitudinal fasciculus (MLF)
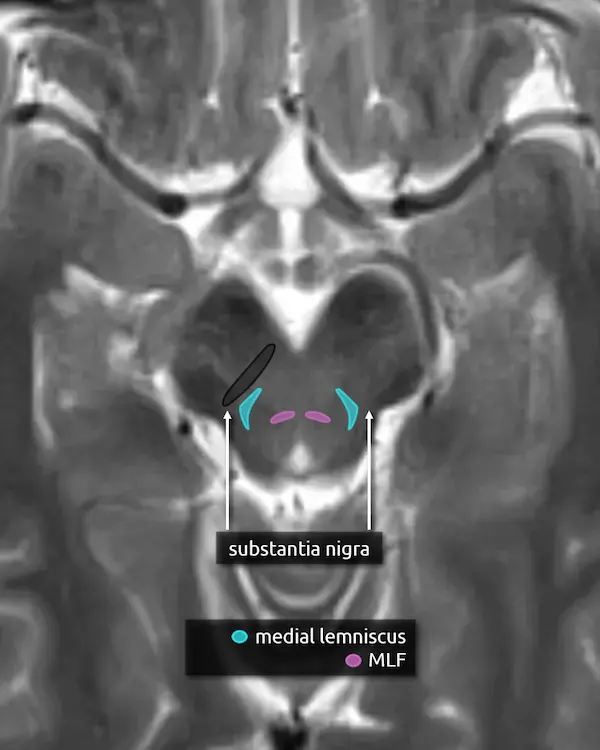

Rostral
Pons
1. Decussation of the superior cerebellar peduncles
2. Superior cerebellar peduncles
3. Corticospinal tracts
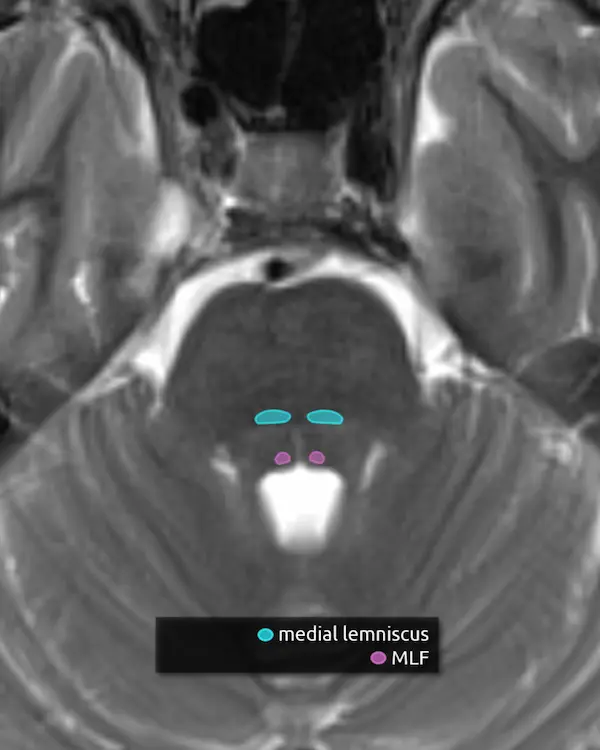
4. Medial lemniscus
5. Medial longitudinal fasciculus (MLF)

Mid
Pons
1. Corticospinal tracts
2. Superior cerebellar peduncles
3. Middle cerebellar peduncles
4. Transverse pontine fibers
5. Medial lemniscus
6. Medial longitudinal fasciculus (MLF)


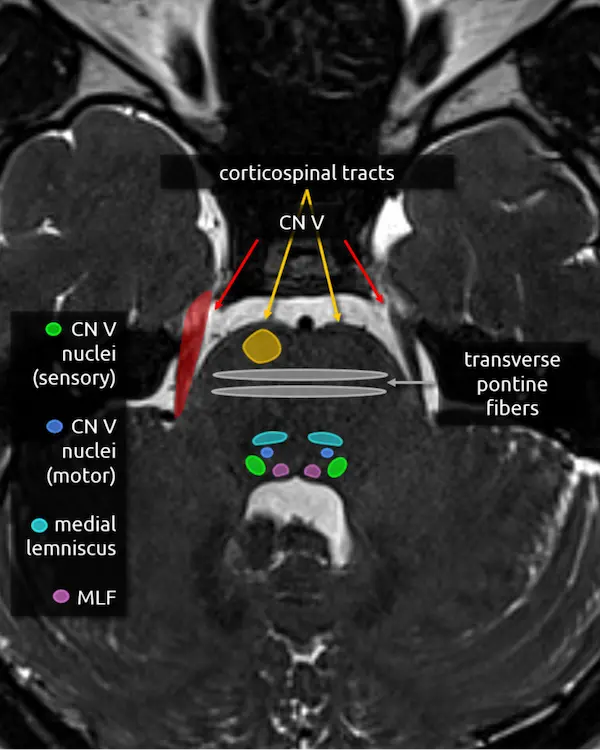
1. Corticospinal tracts
2. Transverse pontine fibers
3. Medial lemniscus
4. Medial longitudinal fasciculus (MLF)
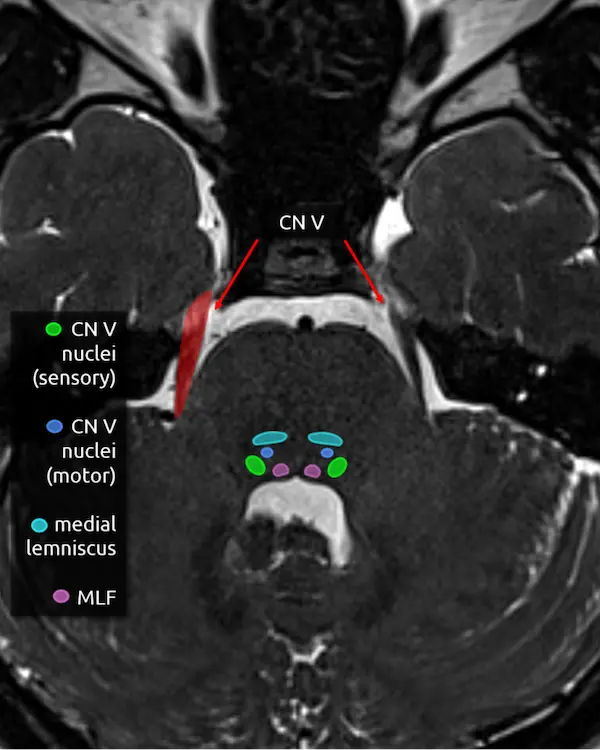
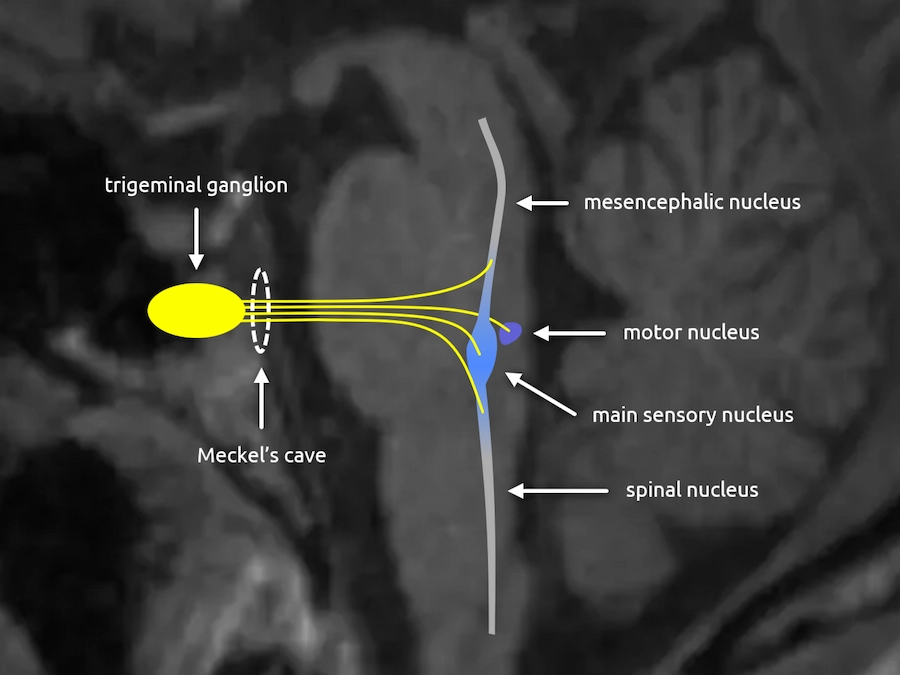
5. Trigeminal nerve (CN V)
The trigeminal nerve is the largest cranial nerve. It exits the side of the pons approximately one slice above the internal auditory canals, then curves forward to traverse the CSF space in front of the pons called the prepontine cistern. It primarily provides sensory innervation to the face, mouth, anterior two thirds of the tongue, nasal sinuses, and dura mater. It has a smaller contribution to motor function of the muscles of mastication.
The trigeminal nerve is large enough to be at least partially visible on routine brain MRIs, though it is sometimes cut off or volume averaged along its course. Notice the image below looks slightly different. This is a heavily T2-weighted sequence with thin slices that is designed to maximize the contrast between CSF and CSF-surrounded structures, usually cranial nerves, blood vessels, or extra-axial lesions. These heavily T2-weighted sequences are useful for ruling out the most common identifiable cause of trigeminal neuralgia: compression by a blood vessel (i.e. neurovascular compression). The region of a cranial nerve most susceptible to symptomatic compression is called the transition zone (aka Obersteiner-Reidlich zone), which is a few millimeters-long gradient of transition from oligodendrocyte myelination (central) to Schwann cells (peripheral). These transition zones are close to where the nerve emerges from the brainstem, called the root entry zone. For the trigeminal nerve, it is 3-4 mm away.
The trigeminal nerve has four nuclei, and two are located around this level.
6. Main sensory nucleus of the trigeminal nerve (CN V)
The main sensory nucleus of the trigeminal nerve is located in the posterolateral pons near the margin of the fourth ventricle approximately one slice above the internal auditory canals.
Lesions in this area will cause ipsilateral sensory loss of the face. A small white matter tract that carries pain and temperature sensation to the body, called the spinothalamic tract (see level 5), is in this region and may be damaged at the same time, resulting in an ipsilateral facial sensory deficit and contralateral body sensory deficit.
7. Motor nucleus of the trigeminal nerve (CN V)
The motor nucleus of the trigeminal nerve is small and located anterior and medial to the main sensory nucleus. As mentioned above, it provides motor innervation to the muscles of mastication primarily, but also to some smaller muscles in the ear and face, for example the tensor tympani muscle and tensor veli palatini.
Damage here may be detectable as weakness and deviation of the mandible or atrophy of the ipsilateral muscles of mastication.
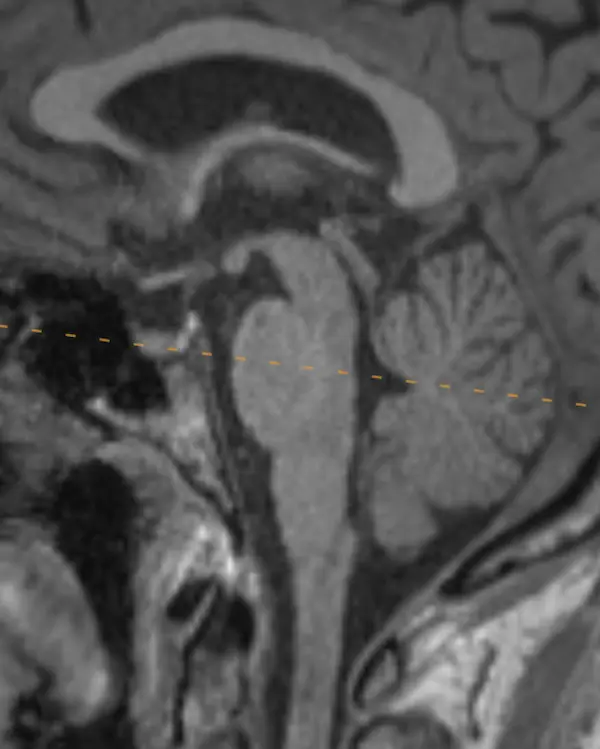
Trigeminal Nerve in Sagittal
The two most important trigeminal nuclei are the main sensory and motor nuclei, introduced above. The mesencephalic and spinal nuclei are elongated and span the majority of the brainstem. Their approximate location in the axial plane will be introduced in the next level.
The name trigeminal comes from its three divisions: ophthalmic (V1), maxillary (V2), and mandibular (V3). This split occurs at the trigeminal ganglion, located in a CSF space beside and below the cavernous sinus called Meckel's cave.
Rostral
Medulla
1. Pyramids
2. Inferior cerebellar peduncles
3. Medial lemniscus
4. Medial longitudinal fasciculus (MLF)
5. Inferior olivary nucleus
The inferior olivary nucleus is located in the upper medulla just posterior to the pyramids. It is involved in motor coordination and is a main component of the dentatorubro-olivary pathway (aka the triangle of Guillain and Mollaret), discussed below. A lesion that damages the predominantly inhibitory interneurons in the tracts connecting the corners of the triangle may result in disinhibition of the inferior olivary nucleus, characteristically but rarely manifesting as palatal myoclonus. Over time, the inferior olivary nucleus may swell, become T2 hyperintense, and eventually atrophy, a process called hypertrophic olivary degeneration.
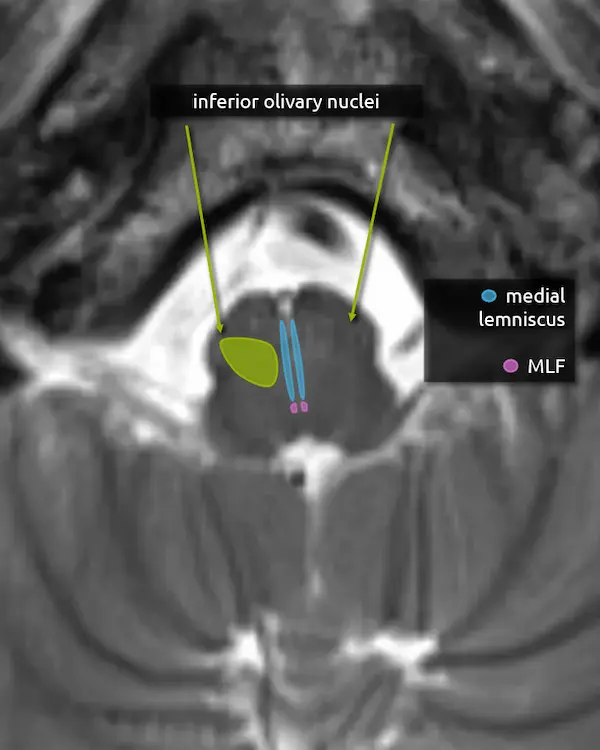
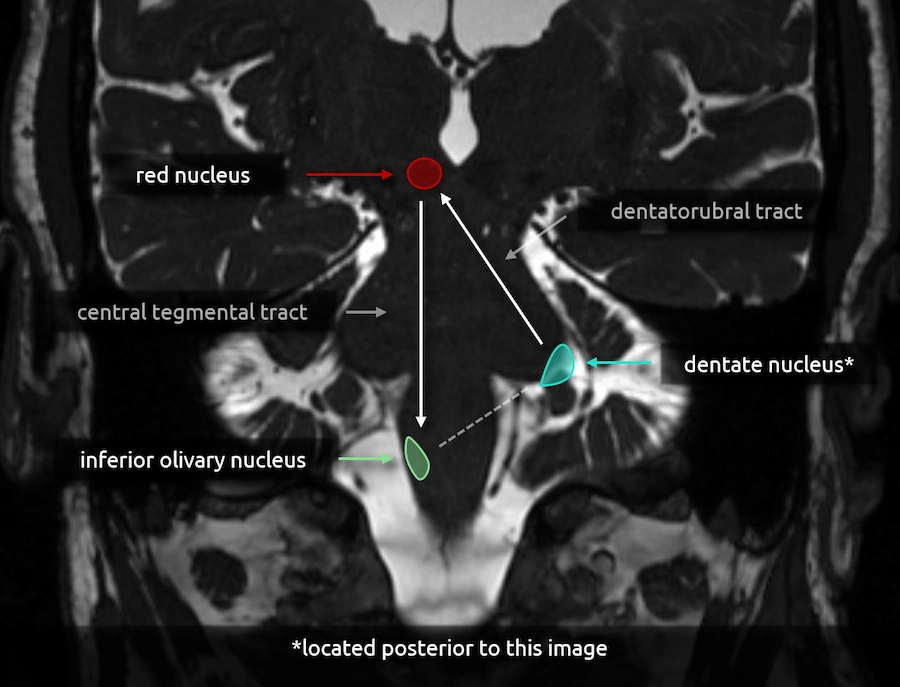
Dentatorubro-Olivary Pathway
(Triangle of Guillain-Mollaret)
The dentatorubro-olivary pathway (aka the triangle of Guillain and Mollaret) forms a triangle with corners at the red nucleus in the midbrain, the inferior olivary nucleus in the medulla, and the contralateral dentate nucleus of the cerebellum.
The red nucleus and ipsilateral olivary nucleus are connected via the descending fibers of the central tegmental tract. The red nucleus and contralateral dentate nucleus are connected via the dentatorubral tract, which travels through the superior cerebellar peduncle.
Note the dotted line between the inferior olivary nucleus and the dentate nucleus. This creates a triangle-like appearance but does not have an anatomic correlate. Fibers from the inferior olivary nucleus do reach the contralateral dentate nucleus, but they take a complicated path through the contralateral inferior cerebellar peduncle and cortex.
Mid
Medulla
1. Pyramids
2. Spinocerebellar tracts
3. Medial lemniscus
4. Medial longitudinal fasciculus (MLF)
Question 1
A patient presents with horizontal diplopia.
a. What structure is likely damaged by this lesion?
b. What syndrome do they likely have?

Question 2
A patient presents with left sided numbness and paresthesias.
a. What structure is likely damaged by this lesion and would explain the patient's symptoms?
Practice Questions
Level 3
Level 4
Midbrain
- Oculomotor nucleus (CN III)
- Edinger-Westphal nucleus
- Oculomotor nerve (CN III)
- Trigeminal (CN V) mesencephalic nucleus
- Trochlear nucleus (CN IV)
- Trochlear nerve (CN IV)
Pons
- Abducens nucleus (CN VI)
- Abducens nerve (CN VI)
- Facial nucleus (CN VII)
- Solitary nucleus
- Spinal nucleus (CN V)
- Facial nerve (CN VII)
Medulla
- Vestibular nucleus (CN VIII)
- Cochlear nucleus (CN VIII)
- Vestibulocochlear nerve (CN VIII)
- Area postrema
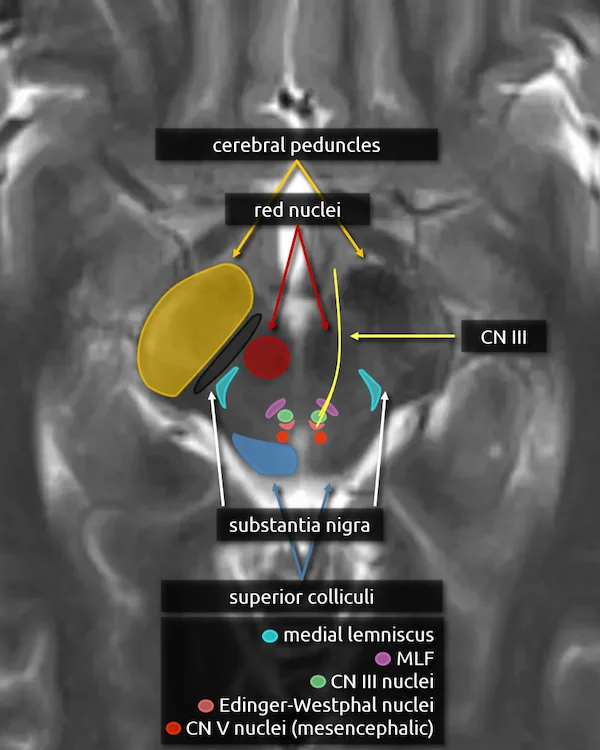
Rostral
Midbrain
1. Cerebral peduncles
2. Superior colliculi
3. Red nucleus
4. Substantia nigra
5. Medial lemniscus
6. Medial longitudinal fasciculus (MLF)
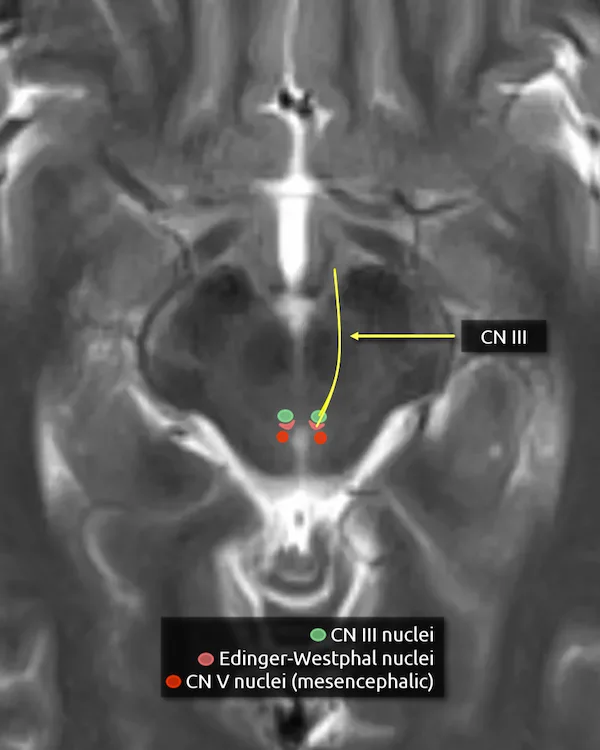
7. Oculomotor nucleus (CN III)
The oculomotor nucleus is located in the upper midbrain posterior to the red nuclei anterior to the cerebral aqueduct. It is one of two nuclei that contributes to the oculomotor nerve. It provides efferent somatic motor fibers.
Lesions involving the oculomotor nucleus are rare but may cause a specific syndrome with bilateral deficits from a unilateral lesion. A single subnucleus spans the midline and supplies the bilateral levator palpebrae muscles, responsible for elevating the eyelids. Additionally, the subnucleus that supplies the superior rectus crosses the midline and supplies both muscles. As a result, nuclear CN III palsy may present with bilateral ptosis and weakness of the bilateral superior rectus muscles. A lesion of solely the nerve fascicle should not cause these symptoms.
8. Edinger-Westphal nucleus
The Edinger-Westphal nucleus is located immediately posterior to the oculomotor nucleus and is the second nucleus that contributes to the oculomotor nerve. It provides parasympathetic motor fibers.
9. Oculomotor nerve (CN III)
The oculomotor nerve exits the brainstem medially after coursing through portions of the red nucleus and substantia nigra. The nerve courses slightly inferior to the axial diagrammatic depiction below, traveling just underneath the mamillary bodies.
Somatic motor innervation:
a. Extraocular muscles (besides the superior oblique and lateral rectus)
b. Levator palpebrae superioris (responsible for elevation of the eyelid)
Parasympathetic motor innervation:
a. Sphincter pupillae muscle (responsible for pupillary constriction)
b. Ciliary body (responsible for light accommodation)
CN III palsy causes the ipsilateral eye to rest in a "down-and-out" position due to unopposed action of the lateral rectus and superior oblique muscles, which are innervated by CN VI and CN IV, respectively. There may also be a unilateral ptosis. The CN III parasympathetic fibers are located on the periphery of the nerve. Because of this, CN III palsy due to compression, e.g., by an aneurysm or a mass, causes a dilated nonreactive pupil. Pupil-sparing CN III palsy is more likely to be due to a medical cause, such as diabetic or hypertensive microangiopathy.
10. Mesencephalic nucleus of the trigeminal nerve (CN V)
The mesencephalic nucleus courses through the midbrain to the mid pons and is involved in proprioception of the structures surrounding the mouth, e.g., the muscles of mastication, temporomandibular joint, teeth, and hard palate.
A not so clinically important factoid that makes this nucleus unique is that axons from this nucleus go directly to target tissues, while other brainstem nuclei first have synapses onto primary sensory neurons in ganglia outside the brainstem (e.g. the trigeminal ganglion, see "trigeminal nerve in sagittal" in level 3). Some fibers from the mesencephalic nucleus also go to the motor nucleus of the trigeminal nerve to mediate bite control and the jaw-jerk reflex.

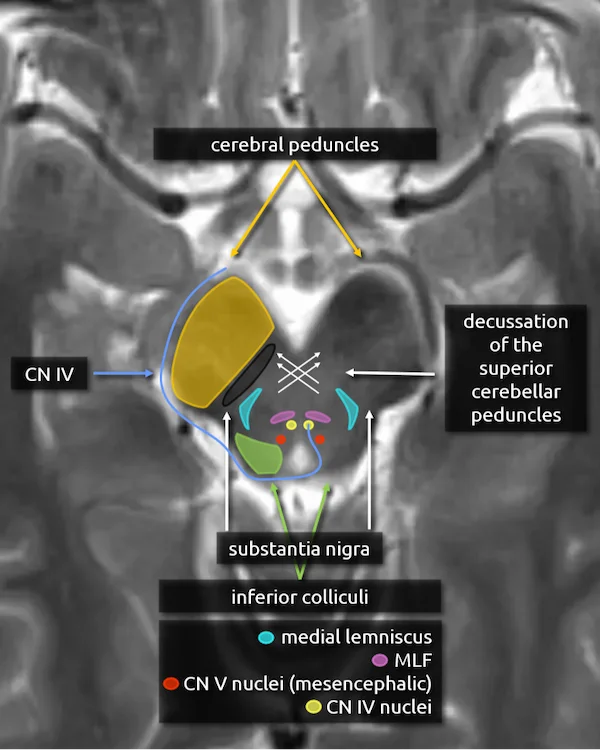
Caudal
Midbrain
1. Cerebral peduncles
2. Inferior colliculi
3. Decussation of the superior cerebellar peduncles
4. Substantia nigra
5. Medial lemniscus
6. Medial longitudinal fasciculus (MLF)
7. Mesencephalic nucleus of the trigeminal nerve (CN V)
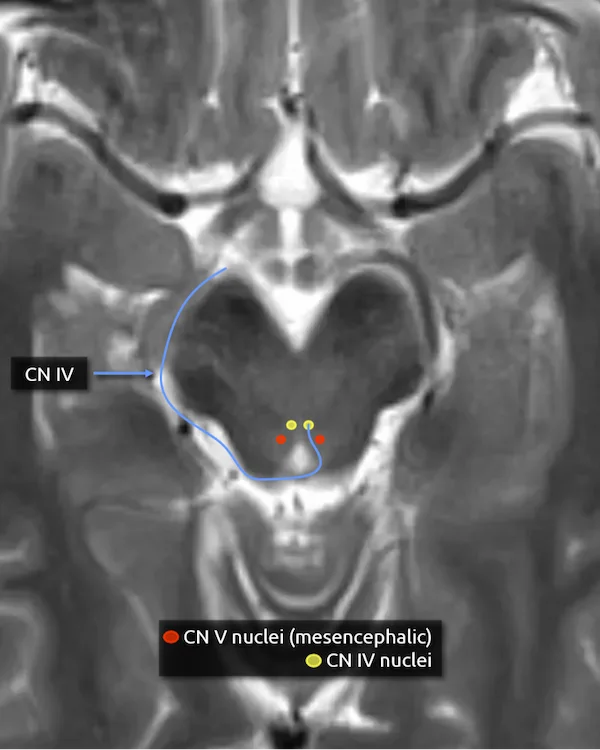
8. Trochlear nucleus (CN IV)
The trochlear nucleus is located in the midbrain at the level of the inferior colliculi just anterior to the cerebral aqueduct. It is approximately in the same location as the oculomotor nucleus (CN III), but one slice lower.
9. Trochlear nerve (CN IV)
The trochlear nerve is very thin and difficult to visualize on routine brain MR. It exits the trochlear nucleus and courses dorsally around the cerebral aqueduct before decussating to the contralateral side of the midbrain. This feature makes it unique among the cranial nerves, as it is the only nerve to cross like this. It is also the only cranial nerve to exit the brainstem dorsally.
The trochlear nerve innervates the contralateral superior oblique muscle, which is primarily responsible for intorsion of the eye.
CN IV palsy presents as vertical diplopia, classically manifesting as difficulty walking down stairs. The patient may compensate by tilting their head to the contralateral side.

Rostral and Mid
Pons
1. Decussation of the superior cerebellar peduncles
2. Superior cerebellar peduncles
3. Corticospinal tracts
4. Medial lemniscus
5. Medial longitudinal fasciculus (MLF)
6. Mesencephalic nucleus of the trigeminal nerve (CN V)
The mesencephalic nucleus of the trigeminal nerve (CN V) continues in a similar location throughout the upper and mid-pons. There are no new structures to introduce at this level, so the images are not included for the sake of brevity. Return to level 3 to review the anatomy of the upper and mid pons.
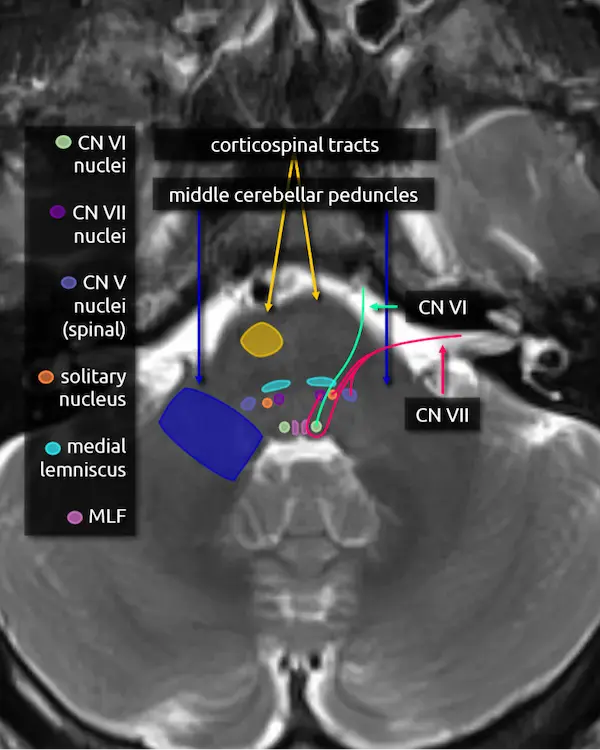
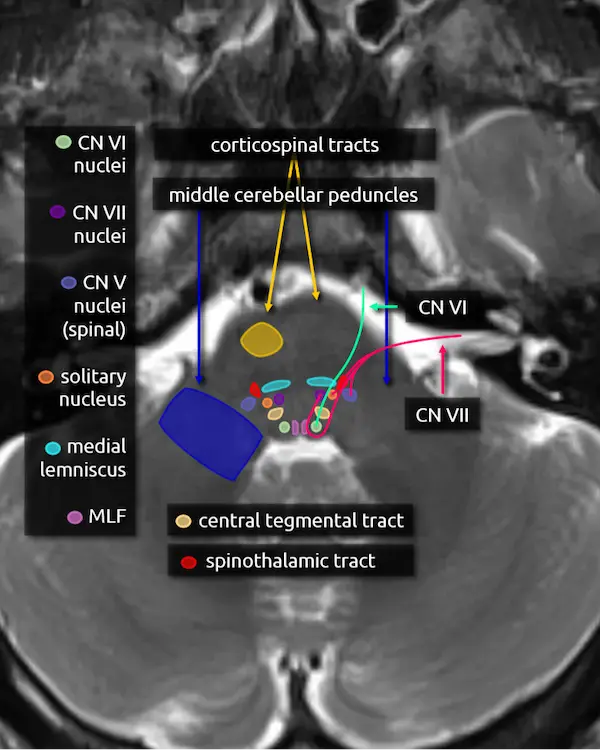
Caudal
Pons
1. Corticospinal tracts
2. Middle cerebellar peduncles
3. Medial lemniscus
4. Medial longitudinal fasciculus (MLF)
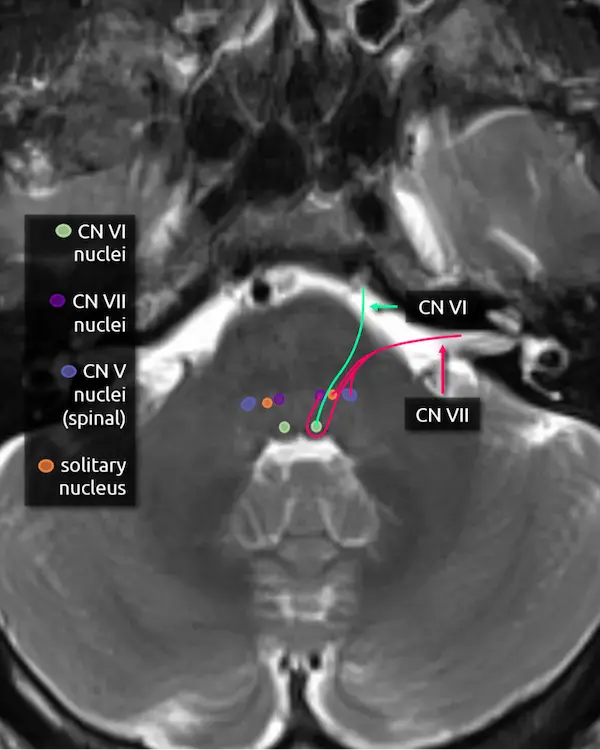
5. Abducens nucleus (CN VI)
The abducens nucleus is located in the dorsal pons at the level of the internal auditory canals. The facial colliculi are the two bumps along the dorsal surface of the pons at this level, which are formed by the facial nerve coursing over the abducens nucleus.
Absence of the abducens nucleus occurs in horizontal gaze palsy with progressive scoliosis (HGPPS), which results in an abnormal contour of the posterior pons due to flattening of the facial colliculi.
6. Abducens nerve (CN VI)
The abducens nerve courses anteriorly from the abducens nucleus and exits the ventral pons at the pontomedullary junction. After traversing the prepontine cistern, the nerve enters Dorello's canal, where it is relatively fixed in place. It also has the longest subarachnoid course of the cranial nerves. These two features make it particularly susceptible to stretching-related injury, e.g., in the setting of brain herniation. After Dorello's canal, the nerve enters the cavernous sinus, where it is susceptible to mass effect from space occupying lesions, e.g., a mass or a cavernous internal carotid artery aneurysm.
The abducens nerve innervates the ipsilateral lateral rectus muscle, responsible for eye abduction. Damage will cause horizontal diplopia.
7. Facial nucleus (CN VII)
The facial nucleus is located in dorsal pons anterior to the abducens nucleus and posterior to the medial lemniscus.
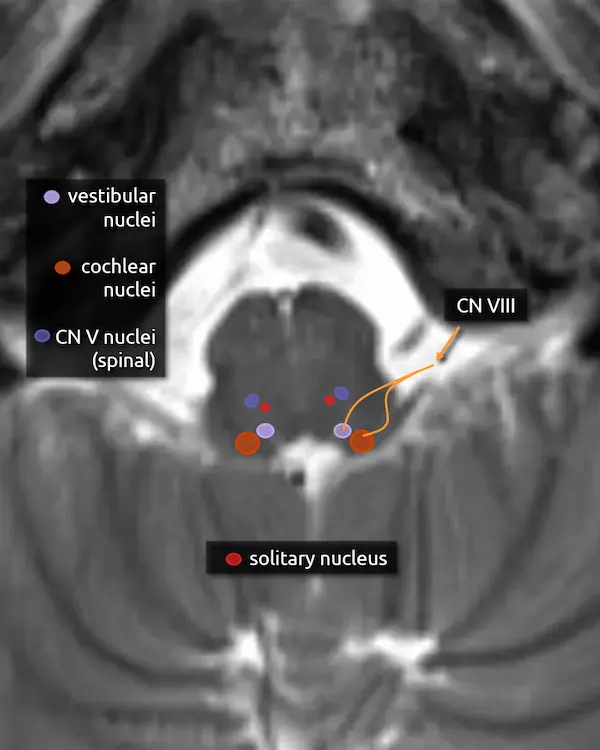
8. Solitary nucleus
The solitary nucleus is located lateral to the facial nucleus in the lower pons and extends to the upper medulla. It contributes to the facial, glossopharyngeal, and vagus nerves.
Damage to the solitary nucleus may manifest as decreased taste sensation on the ipsilateral tongue.
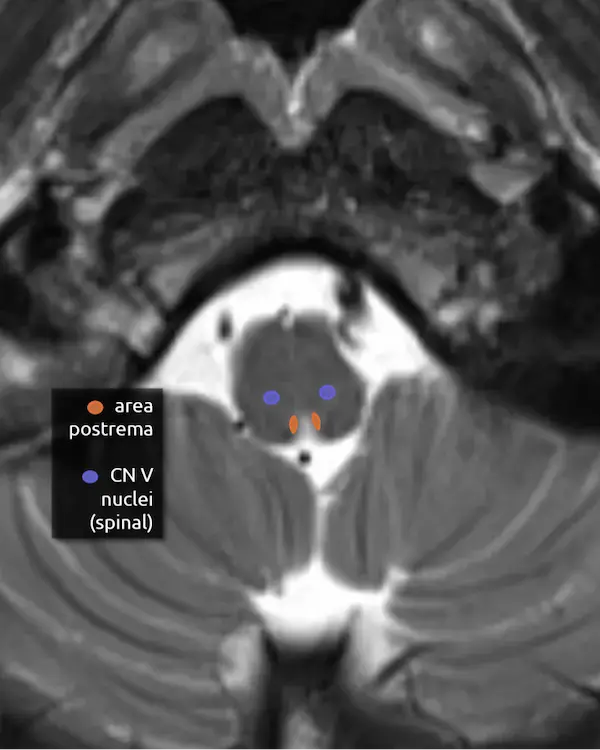
9. Spinal nucleus of the trigeminal nerve (CN V)
The spinal nucleus of the trigeminal nerve is the inferior continuation of the main sensory nucleus of the trigeminal nerve (see level 3). It is involved in sensation of the head and face. It receives afferent fibers from the facial, glossopharyngeal, and vagus nerves.
10. Facial nerve (CN VII)
The facial nerve courses posteriorly from the facial nucleus before looping over the ipsilateral abducens nucleus and exiting the anterolateral pons at the pontomedullary junction. It then enters the internal auditory canal with the vestibulocochlear nerve (CN VIII). Four nuclei contribute to the facial nerve; the three listed above, and a fourth called the superior salivary nucleus responsible for parasympathetic fibers located medial to the facial nucleus, not pictured here. The nerve has motor, sensory, and parasympathetic functions:
Motor:
a. Face (muscles of expression)
b. Stylohyoid, stapedius, posterior belly of the digastric muscle
Sensory:
a. Taste (anterior 2/3 of tongue, floor of mouth, palate)
b. Somatic sensation (posterior EAC, mastoid, lateral pinna)
Parasympathetic:
a. Salivary glands (submandibular sublingual)
Similar to the trigeminal nerve, the facial nerve may become irritated by nearby blood vessels (neurovascular compression syndrome), manifesting as hemifacial spasm.
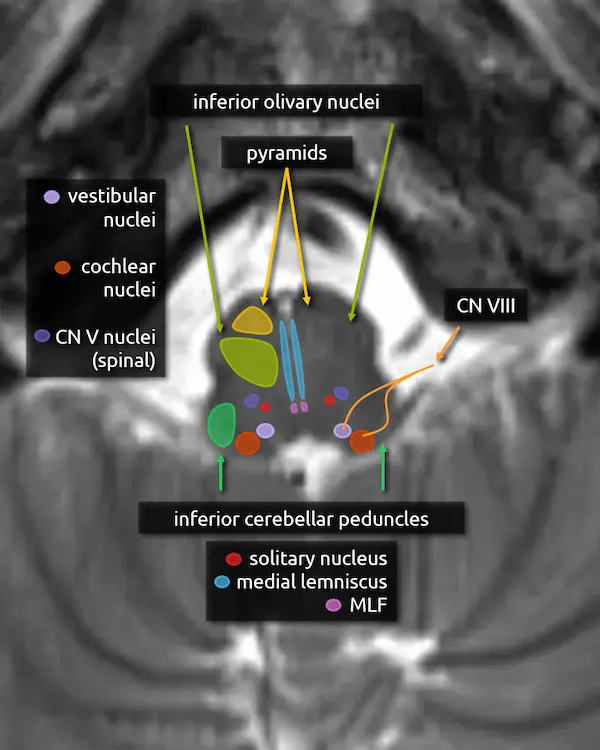
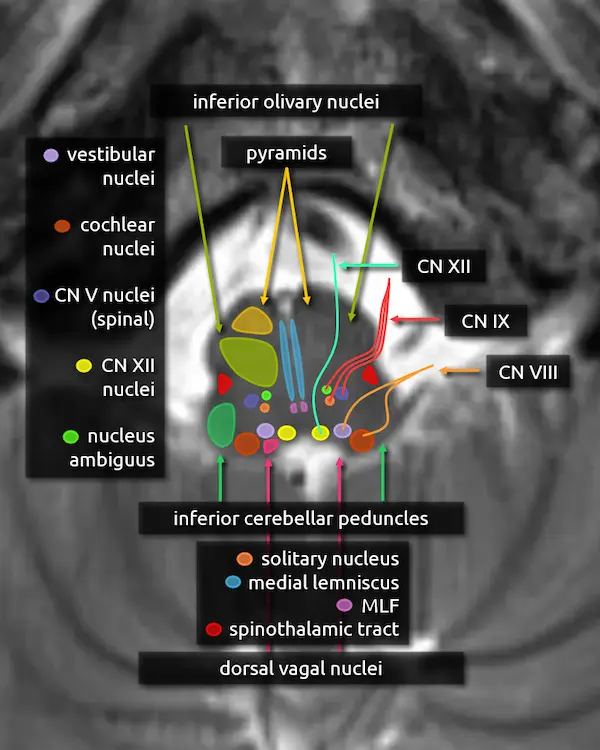
Rostral
Medulla
1. Pyramids
2. Inferior cerebellar peduncles
3. Medial lemniscus
4. Medial longitudinal fasciculus (MLF)
5. Spinal nucleus of the trigeminal nerve (CN V)
6. Solitary nucleus
5. Vestibular nuclei (CN VIII)
The vestibular nuclei are a complex of four cell groups located mostly in the dorsal medulla with some extension to the lower pons. The receive information from the inner ear and are responsible for balance, posture, and eye movement in response to head motion.
6. Cochlear nucleus (CN VIII)
The cochlear nuclei are a complex of two cell groups located in the dorsal medulla. They receive information from the inner ear and are responsible for hearing.
7. Vestibulocochlear nerve (CN VIII)
The vestibulocochlear nerve is formed by fibers of the vestibular and cochlear nuclei. It exits the pontomedullary junction lateral and slightly inferior to the facial nerve before entering the internal auditory canal.
The most common mass in the cerebellopontine angle is a vestibular schwannoma, i.e., a schwannoma arising from the vestibular component of CN VIII. Due to its long course through the subarachnoid space, CN VIII is the most commonly involved cranial nerve in superficial siderosis, which manifests as sensorineural hearing loss. The facial nerve, with its similar course, is the second most commonly involved. Similar to the trigeminal and facial nerves, CN VIII may become irritated by nearby blood vessels, manifesting as intermittent vertigo (vestibular paroxysmia).
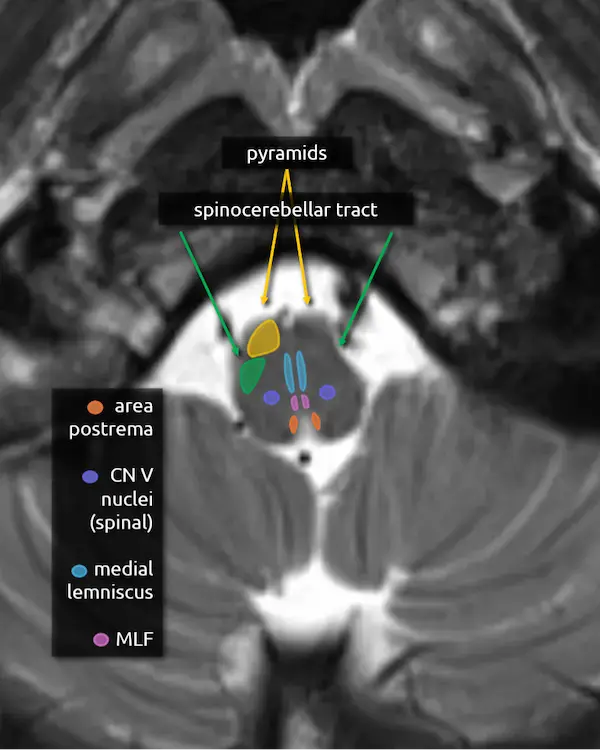
Mid
Medulla
1. Pyramids
2. Spinocerebellar tracts
3. Medial lemniscus
4. Medial longitudinal fasciculus (MLF)
5. Spinal nucleus of the trigeminal nerve (CN V)
6. Area postrema
The area postrema is in the medial dorsal medulla along the floor of the fourth ventricle and median aperture. It is one of several circumventricular organs (CVOs) that do not have a blood-brain barrier. CVOs can be divided into secretory (e.g. secrete hormones) or sensory (e.g. sense hormones and toxins in the CSF). The area postrema is sensory, responsible for detecting toxins and inducing vomiting.
Signal abnormality in the area postrema is a characteristic feature of neuromyelitis optica spectrum disorder (NMOSD). Damage to this area, either in NMOSD or from other conditions, can cause area postrema syndrome, characterized by nausea, vomiting, and sometimes hiccups.
Question 1
a. What structures are likely damaged by this lesion?
b. What is this syndrome called?
Practice Questions
Level 4
Question 2
A patient presents with horizontal gaze palsy since birth.
a. What section of the brainstem predominantly has an abnormal contour: the midbrain, pons, or medulla?
b. Damage or congenital absence of what nucleus in the pons would produce horizontal gaze palsy?


Midbrain:
Oculomotor nuclei (CN III)Edinger-Westphal nuclei (CN III)Oculomotor nerve (CN III)Trigeminal mesencephalic nucleus (CN V)Trochlear nucleus (CN IV)Trochlear nerve (CN IV)Level 5
Midbrain
- Cerebral peduncles: (somatotopy, corticospinal and corticobulbar tracts, and corticopontocerebellar pathway)
- Spinothalamic tract
- Ventral tegmental area (VTA)
- Basis, tegmentum, tectum
- Raphe nuclei
Pons
- Locus ceruleus
- Central tegmental tract
- Pontine lesion symptom map
Medulla
- Hypoglossal nuclei
- Hypoglossal nerve (CN XII)
- Nucleus ambiguus
- Glossopharyngeal nerve (CN IX)
- Dorsal vagal nuclei
- Nucleus gracilis
- Nucleus cuneatus
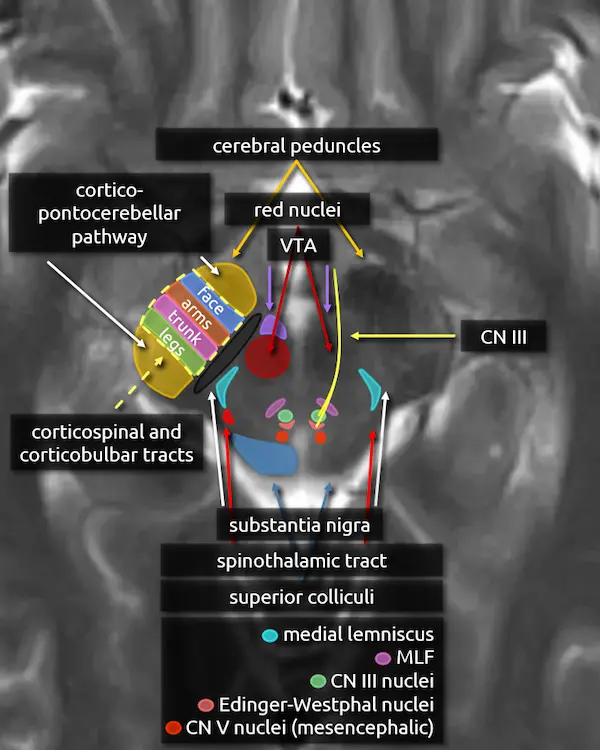
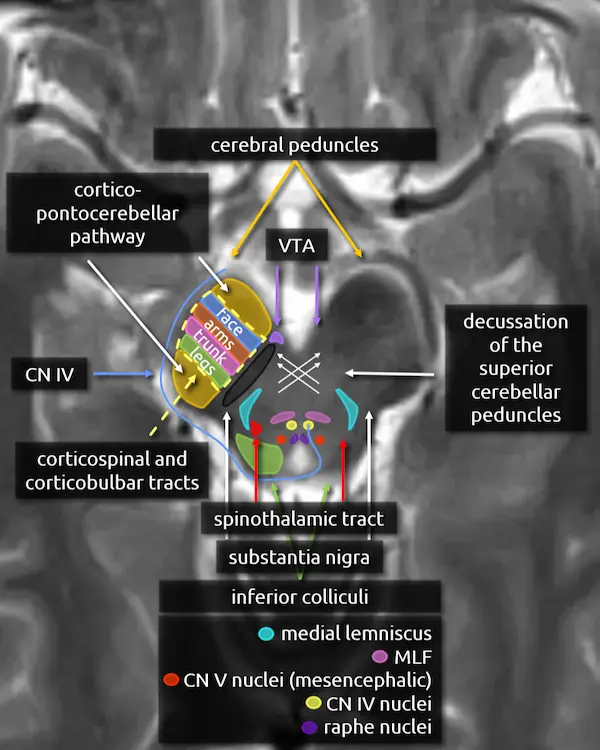
Rostral
Midbrain
1. Cerebral peduncles
2. Superior colliculi
3. Red nucleus
4. Substantia nigra
5. Medial lemniscus
6. Medial longitudinal fasciculus (MLF)
7. Oculomotor nucleus (CN III)
8. Edinger-Westphal nucleus
9. Oculomotor nerve (CN III)
10. Mesencephalic nucleus of the trigeminal nerve (CN V)
11. Cerebral peduncles (expanded)
The corticospinal and corticobulbar tracts run through the middle third of the cerebral peduncle. Fibers are organized somatotopically; the most anteromedial part innervates the muscles of the face (corticobulbar tract) followed by the arms, trunk, and legs moving posterolateral.
The anterior and posterior thirds of the cerebral peduncle contain tracts of the corticopontocerebellar pathway. Tracts in the anterior component originate in the frontal lobe (frontopontine fibers) and tracts in the posterior component originate from the temporal lobe (temporopontine fibers).
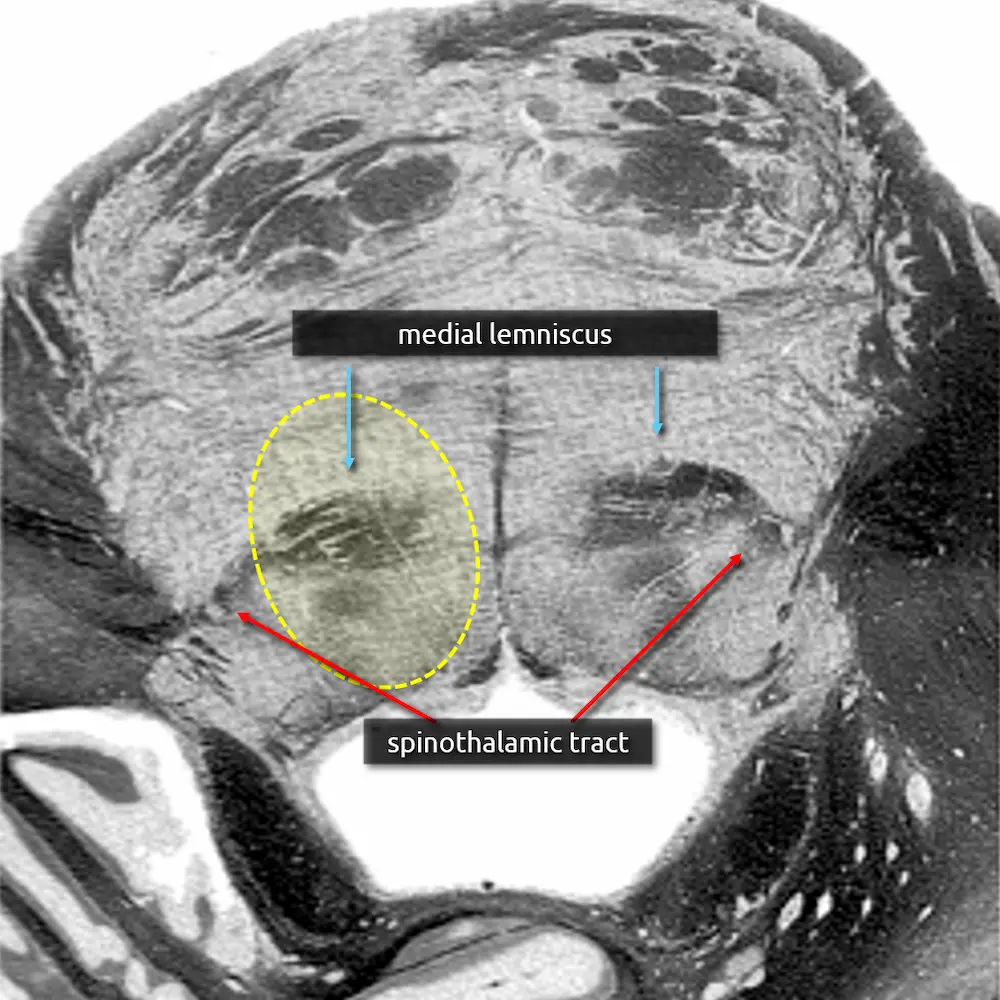
12. Spinothalamic tract
The spinothalamic tract is responsible for pain and temperature sensation. It is found throughout the dorsal brainstem adjacent to the medial lemniscus. Like the medial lemniscus, fibers terminate at the thalamic ventral posterolateral nucleus (VPL).
Fibers of the spinothalamic tract decussate in the spinal cord, so lesions will cause contralateral loss of pain and temperature sensation.
13. Ventral tegmental area (VTA)
The ventral tegmental area (VTA) contains dopaminergic neurons that are involved in reward and goal-directed behaviors. It is found in the medial ventral midbrain in a region called the midbrain tegmentum, introduced below.
Dysfunction of the dopaminergic neurons in the VTA have been implicated in the pathophysiology of addiction, schizophrenia, and depression.
.webp)

Brainstem Divisions:
The Basis, Tegmentum, and Tectum
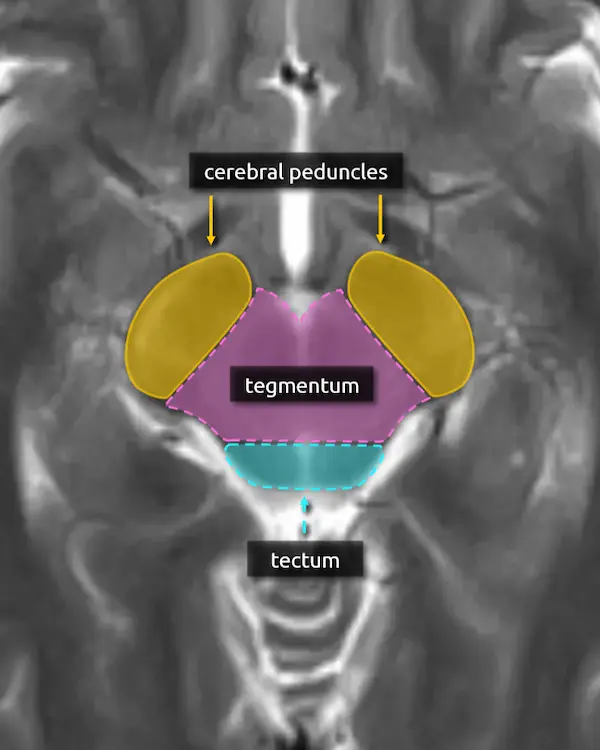
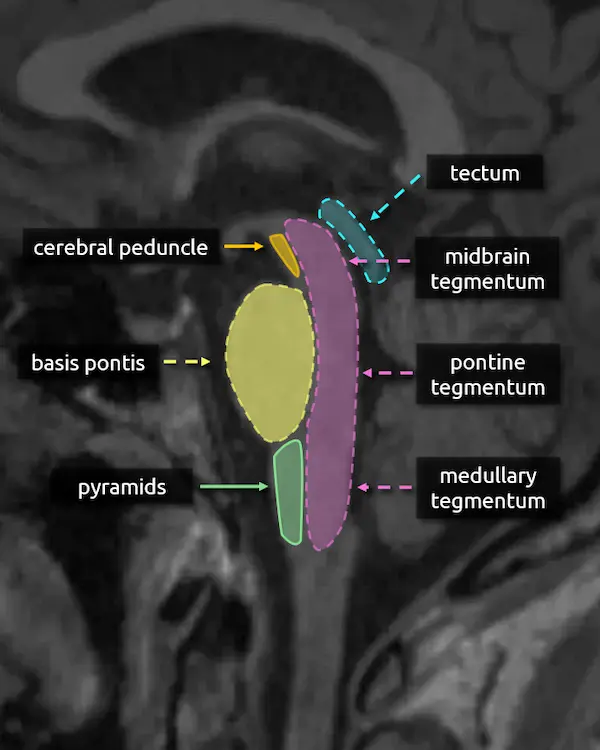
The brainstem can also be divided up into the basis, tegmentum, and tectum.
The basis, or base, simply refers to the anterior portion of the brainstem, which contains predominantly white matter tracts. In the midbrain, this corresponds to the cerebral peduncle. In the pons, it corresponds to the basis pontis; the bulbous part containing the transverse pontine fibers, corticospinal tract, etc. In the medulla, it corresponds to the pyramids.
The tegmentum is the central part of the brainstem. It contains the majority of the brainstem nuclei, including of the cranial nerves and structures of the reticular formation. Like the basis, there are white matter tracts that run through the tegmentum, some of which have been covered here. For example, recall the central tegmental tract, introduced in level 4 in reference to the triangle of Guillain-Mollaret, whose name should make more sense now, and the medial lemniscus.
The tectum is only located in the midbrain and is yet another way to refer to the superior and inferior colliculi (recall "quadrigeminal plate").
Caudal
Midbrain
1. Cerebral peduncles
2. Inferior colliculi
3. Decussation of the superior cerebellar peduncles
4. Substantia nigra
5. Medial lemniscus
6. Medial longitudinal fasciculus (MLF)
7. Mesencephalic nucleus of the trigeminal nerve (CN V)
8. Trochlear nucleus (CN IV)
9. Trochlear nerve (CN IV)
10. Cerebral peduncles (expanded)
11. Spinothalamic tract
12. Ventral tegmental area (VTA)
13. Raphe nuclei
There are seven groups of neurons that comprise the raphe nuclei spanning the midline from the lower midbrain to the medulla. The largest is located in the midbrain, sends connections to the forebrain, and is called the dorsal raphe nucleus. The remaining raphe nuclei in the pons and medulla are not pictured, but they are located in a similar position along the midline. The raphe nuclei are responsible for producing serotonin which is involved in mood, sleep, and memory.
Dysfunction of the serotonergic neurons and the connections between the raphe nuclei are strongly implicated in the pathogenesis of depression.


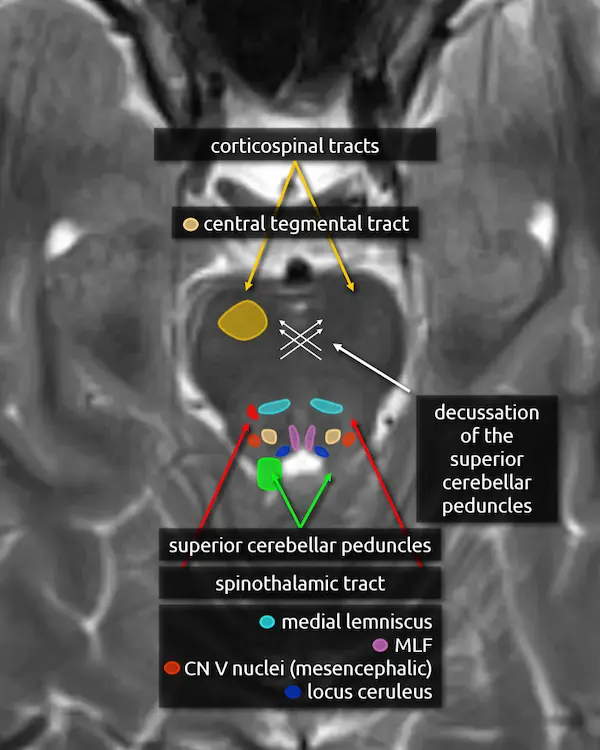
Rostral
Pons
1. Decussation of the superior cerebellar peduncles
2. Superior cerebellar peduncles
3. Corticospinal tracts
4. Medial lemniscus
5. Medial longitudinal fasciculus (MLF)
6. Mesencephalic nucleus of the trigeminal nerve (CN V)
7. Spinothalamic tract
8. Locus ceruleus
The locus ceruleus is located in the posteromedial aspect of the upper pons and means "blue spot," named due to its pigmented appearance. It contains noradrenergic neurons responsible for producing norepinephrine. Additional noradrenergic neurons similar to those in the locus ceruleus are located in the lateral tegmentum of the pons and medulla (lateral tegmental area). Together, these regions supply norepinephrine to both the brain and spinal cord involved in a variety of functions, notably arousal, attention, and blood pressure control.
9. Central tegmental tract
The central tegmental tract extends from the midbrain to the medulla but is easiest to approximate in the dorsal pons. It connects the red nucleus to the ipsilateral inferior olivary nucleus (see the dentatorubro-olivary pathway).
Signal abnormalities of the central tegmental tract may occur with vigabatrin toxicity, which is common in children being treated for infantile spasms. Lesions here may also cause hypertrophic olivary degeneration, classically associated with palatal myoclonus.


Caudal
Pons
1. Corticospinal tracts
2. Middle cerebellar peduncles
3. Medial lemniscus
4. Medial longitudinal fasciculus (MLF)
5. Abducens nucleus (CN VI)
6. Abducens nerve (CN VI)
7. Facial nucleus (CN VII)
8. Solitary nucleus
9. Spinal nucleus of the trigeminal nerve (CN V)
10. Facial nerve (CN VII)
11. Spinothalamic tract
12. Central tegmental tract

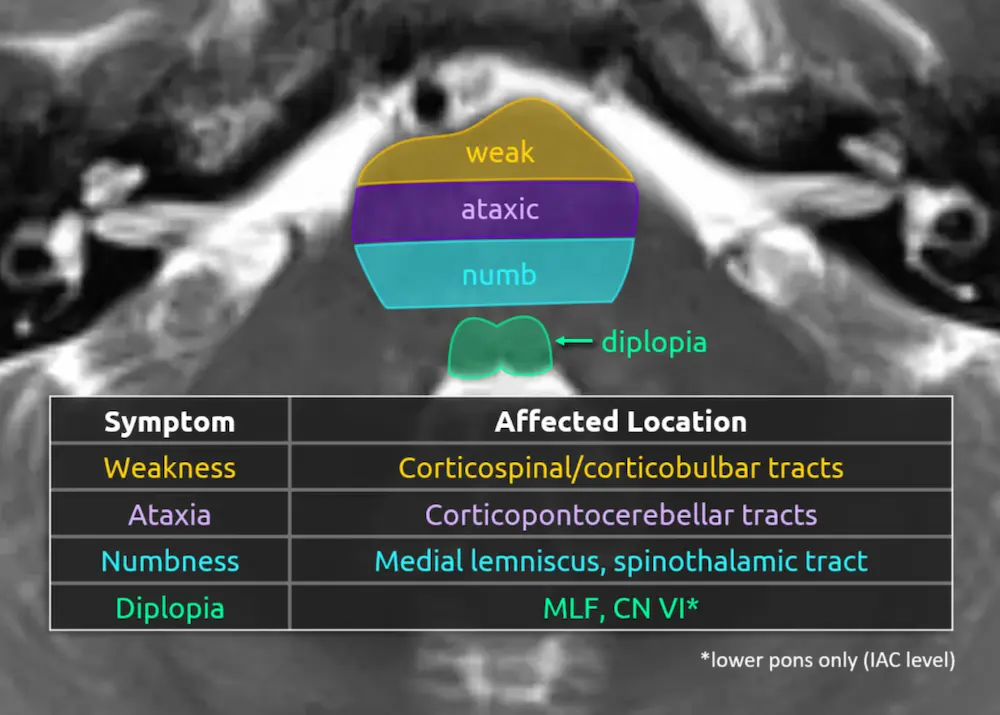
Predicting deficits of a pontine lesion
You now know enough pontine anatomy to predict the most likely symptoms for a lesion anywhere in the majority of the pons. See the figure on the right for a simplified but practical way of conceptualizing this anatomy.
Lesions in the anterior aspect of the pons are likely to damage the corticospinal and corticobulbar tracts, producing weakness or paralysis. Lesions in the center of the pons are likely to damage the transverse pontine fibers, causing ataxia. Remember that the corticopontocerebellar pathway makes up a large part of those fibers. Lesions towards the back of the pons are likely to involve the medial lemniscus and spinothalamic tract, producing sensory deficits. Lesions that involve the most posterior aspect of the pons surrounding the fourth ventricle are likely to cause diplopia due to damage to the MLF and/or the abducens nerve (CN VI), depending on the level.
Rostral
Medulla
1. Pyramids
2. Inferior cerebellar peduncles
3. Medial lemniscus
4. Medial longitudinal fasciculus (MLF)
5. Spinal nucleus of the trigeminal nerve (CN V)
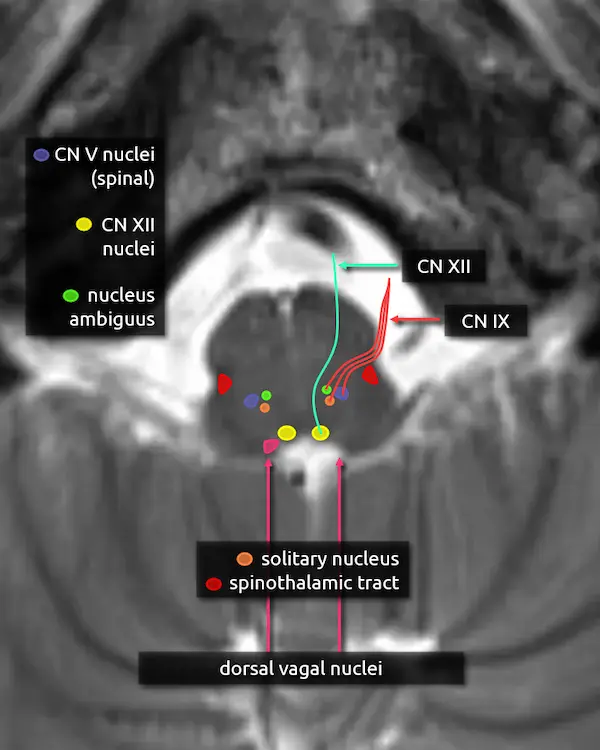
6. Hypoglossal nucleus (CN XII)
The hypoglossal nucleus is located in the dorsal medulla near the midline. It is elongated in the craniocaudal dimension, with extension towards the mid medulla approximately to the most inferior aspect of the fourth ventricle, called the obex. For imaging purposes, the obex is essentially the inferior tip of the median aperture. In reality, they are separate structures.
7. Hypoglossal nerve (CN XII)
The hypoglossal nerve travels anteriorly from the hypoglossal nucleus and exits the ventral medulla. From there, it traverses the premedullary cistern and enters the hypoglossal canal of the occipital bone. It innervates the muscles of the tongue besides the palatoglossus muscle, which is innervated by the vagus nerve (CN X).
Hypoglossal nerve palsy may cause weakness of the ipsilateral tongue musculature, eventually causing atrophy of the musculature which may be seen on imaging. On physical exam, the tongue may deviate towards the paralyzed side during protrusion.
8. Nucleus ambiguus
The nucleus ambiguus is located primarily in the upper medulla just dorsal to the inferior olivary nucleus. It is a motor nucleus that receives fibers from the corticobulbar tract and provides fibers to the glossopharyngeal nerve (CN IX), vagus nerve (CN X), and spinal accessory nerve (CN XI). It innervates muscles of the pharynx and larynx, primarily involved in swallowing and speech.
Lesions of the nucleus ambiguus may cause dysphagia and hoarseness.
9. Glossopharyngeal nerve (CN IX)
The glossopharyngeal nerve exits the lateral aspect of the upper medulla before coursing slightly inferiorly and entering the jugular foramen of the skull base. It has sensory, motor, and parasympathetic functions provided by four nuclei:
Sensory
a. Solitary nucleus: taste from posterior 1/3 of the tongue
b. Spinal nucleus of the trigeminal nerve: somatic sensation to the posterior 1/3 of the tongue, pharynx, middle, ear, and tonsils.
Motor
a. Nucleus ambiguus: stylopharyngeus muscle, responsible for elevation of the pharynx during speech and swallowing.
Parasympathetic
a. Inferior salivary nucleus (not pictured): small nucleus in the lower pons superomedial to the nucleus ambiguus. It innervates the parotid gland.
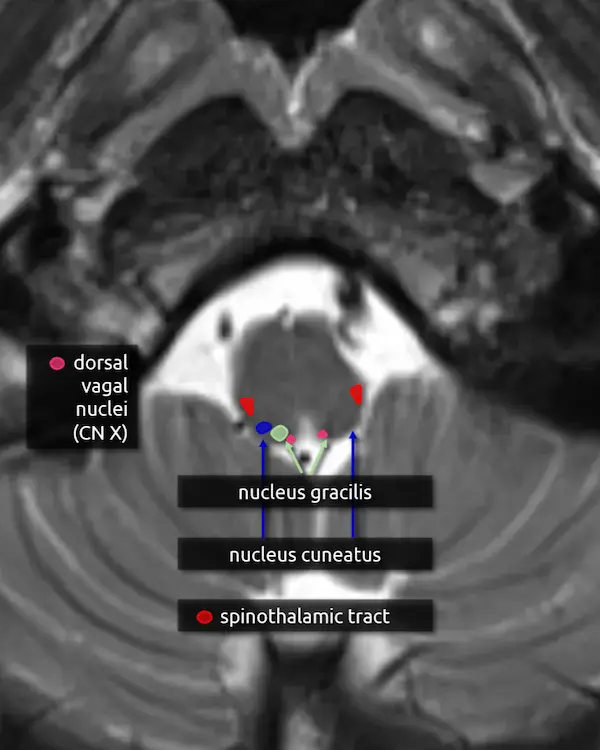
10. Dorsal vagal nuclei (CN X)
The dorsal vagal nuclei are elongated and located in the majority of the dorsal medulla posterolateral to the hypoglossal nucleus. It mainly provides parasympathetic innervation to several visceral organs in the chest and abdomen.
11. Vagus nerve (CN X)
The vagus nerve exits the lateral brainstem just below the glossopharyngeal nerve (CN IX) and follows a similar course. Four nuclei contribute to the nerve: the dorsal vagal nucleus, nucleus ambiguus, solitary nucleus, and spinal nucleus of the trigeminal nerve.
Mid
Medulla
1. Pyramids
2. Spinocerebellar tracts
3. Medial lemniscus
4. Medial longitudinal fasciculus (MLF)
5. Spinal nucleus of the trigeminal nerve (CN V)
6. Area postrema
7. Dorsal vagal nuclei (CN X)
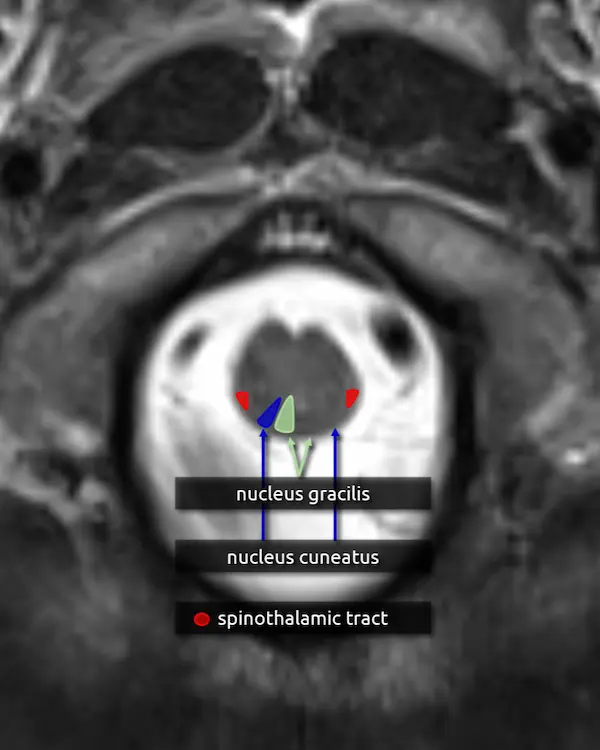
8. Nucleus gracilis and cuneatus
Nucleus gracilis:
a. Located in the medial dorsal mid to lower medulla. It receives sensory input from the lower body (lower trunk, lower limbs) from T7 and below.
Nucleus cuneatus:
a. Located lateral to the nucleus gracilis. It receives sensory input from the upper body (upper trunk, neck, upper limbs) from T6 and above.
First order neurons carrying vibration, fine touch, and proprioception information from the spinal cord synapse with second order neurons in the nucleus gracilis and cuneatus. Second order neuron axons then decussate and travel superiorly through the medial lemniscus before reaching the third order neurons in the ventral posterolateral nucleus (VPL) of the thalamus. Collectively, this is called the dorsal column medial lemniscus (DCML) pathway.
Caudal
Medulla
1. Pyramids
2. Pyramidal decussation
3. Nucleus gracilis
4. Nucleus cuneatus
Question 1
A 10-month-old girl with a history of infantile spasms gets a follow-up MRI.
a. What brainstem structure is abnormally bright?
Practice Questions
Level 5
Question 2
An immunosuppressed patient presents with left trigeminal nerve palsy and difficulty swallowing.
a. What structures in the pons are likely damaged that could explain the patient's presentation?
b. What structure in the medulla are likely damaged that could explain the patient's presentation?


Question 3
A patient presents with loss of pain and temperature sensation of the body on the left, loss of pain and temperature sensation of the face on the right, and vertigo. On further investigation, they also have difficulty speaking and swallowing.
a. What structures are damaged that could explain these symptoms?
b. What is the name of this syndrome?
References
- Blumenfeld H. Neuroanatomy through Clinical Cases. Third Edition: Oxford, New York: Oxford University Press; 2021. 1056 p.
- Hurley RA, Flashman LA, Chow TW, Taber KH. The Brainstem: Anatomy, Assessment, and Clinical Syndromes. JNP. 2010 Jan;22(1):iv–7.
- Shepherd TM, Ades-Aron B, Bruno M, Schambra HM, Hoch MJ. Direct In Vivo MRI Discrimination of Brain Stem Nuclei and Pathways. American Journal of Neuroradiology. 2020 Apr 3.
- Sciacca S, Lynch J, Davagnanam I, Barker R. Midbrain, Pons, and Medulla: Anatomy and Syndromes. RadioGraphics. 2019 July;39(4):1110–25.
- Bae YJ, Kim JM, Sohn CH, Choi JH, Choi BS, Song YS, et al. Imaging the Substantia Nigra in Parkinson Disease and Other Parkinsonian Syndromes. Radiology. 2021 Aug;300(2):260–78.
- Basile GA, Quartu M, Bertino S, Serra MP, Boi M, Bramanti A, et al. Red nucleus structure and function: from anatomy to clinical neurosciences. Brain Struct Funct. 2021 Jan 1;226(1):69–91.
- Lim CY, Seo Y, Sohn B, Seong M, Kim ST, Hong S, et al. The Inferior Cerebellar Peduncle Sign: A Novel Imaging Marker for Differentiating Multiple System Atrophy Cerebellar Type from Spinocerebellar Ataxia. American Journal of Neuroradiology. 2025 June 1;46(6):1223–30.
- Terrier LM, Hadjikhani N, Destrieux C. The trigeminal pathways. J Neurol. 2022 July 1;269(7):3443–60.